
advertise here
Original Article
A Retrospective Study On Maternal Deaths And Its Causes In A
Tertiary Care Teaching Institute In Northern Telangana.
Year : 2019 | Volume : 7 | Issue : 2 Page : 71-74
Background:
Maternal mortality is a strong indicator for measuring the health care provided to the women by any society. Although pregnancy is considered physiological at times it leads to morbidity and even death. The aim of the study is to evaluate various epidemiological factors, causes of maternal mortality and to determine the preventable factors associated with maternal deaths.
Method:
A retrospective hospital based study was conducted in the Department of OBG, Prathima Institute of Medical Sciences, A tertiary care hospital in Karimnagar, Telangana State, India, over a period of 10 years from Jan 2009 to Dec 2018.
Results:
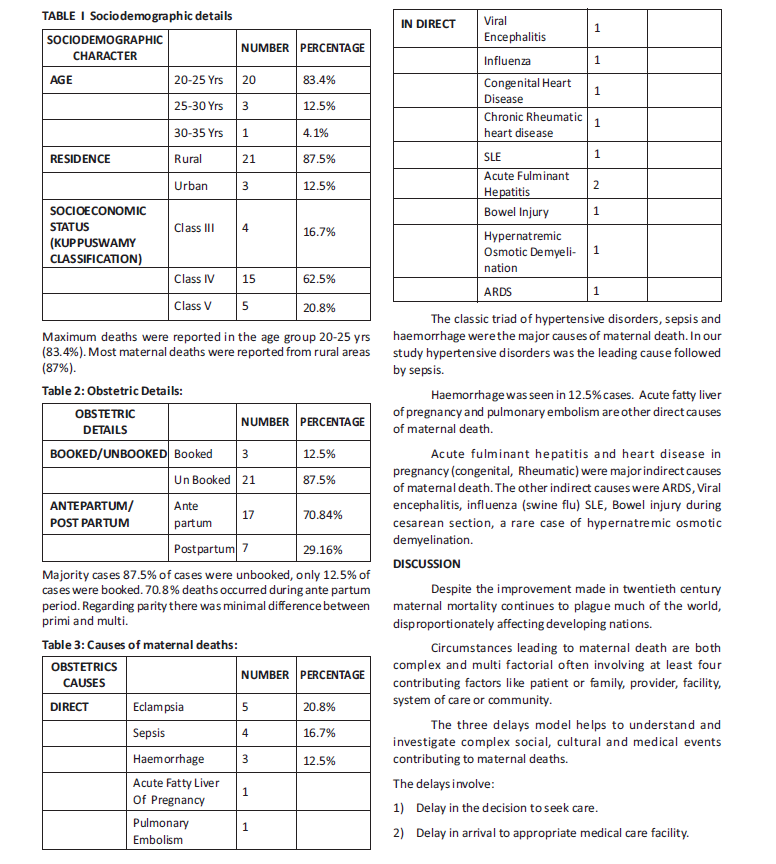
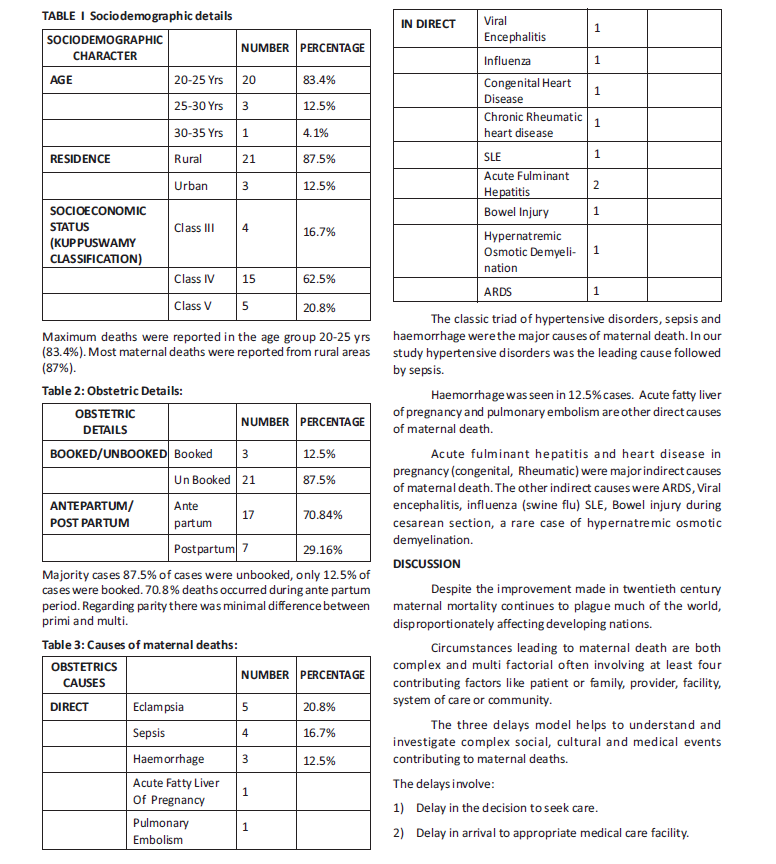
A total of 24 deaths were analysed. Maximum number of deaths were seen in age group 20-24 years, More deaths were seen in ante partum period (70.84%) than post partum period (29.16%). Most of them were unbooked (87.5%). than booked cases (12.5%). The classic triad of hypertensive disorders (20.8%) Sepsis (16.7%) and Haemorrhage (12.5%) were the major direct causes. Hepatitis, Heart disease in pregnancy, Respiratory disease are the common indirect causes.
Conclusion:
Majority of deaths were preventable by proper antenatal care, early detection of high risk pregnancies and timely referral to higher centre.
Keywords: Maternal mortality, Eclampsia, Haemorrhage, Sepsis, Maternal mortality ratio.
INTRODUCTION Globally maternal mortality has been falling with substantial variation among countries and within countries (1,2). The MMR was 216 maternal deaths/ 1Lakh live births in 2015 globally (1, 2, 3).country specific MMR estimates ranged from 3 (Finland) to 1360 (Sierra leone) maternal deaths/1Lakh live births.
The need for continued efforts to eliminate preventable maternal deaths is highlighted by the gap between the sustainable development goal of fewer than 70 maternal deaths/1Lakh live births globally by 2030, and recent MMR of low performing regions, which is nearly 20 times the goal MMR.
Maternal death can be defined as the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of pregnancy, from any cause related to aggravated by the pregnancy or its management but not from accidental or incidental causes.(4) A direct obstetric death results from obstetric complications of pregnancy, delivery or the post partum period and from interventions, omissions, incorrect treatment or a chain of events related to the obstetric complication (3) An indirect obstetric death results from pre-existing disease (Eg: diabetis, cardiac disease, malaria, tuberculosis, HIV) or new disease that develops during pregnancy and is unrelated to pregnancy but is aggravated by the physiologic effects of pregnancy (Eg: Influenza) India has ground breaking progress in recent years in reducing MMR by 77% from 556 per 1lakh live births in 1990 to 130 per 1lakh live births in 2016 (5, 7) India’s present MMR is below the millennium development goal (MDG) (6) target and puts the country on track to achieve the sustainable development goal (SDG). Kerala has MMR of 46, while Assam has MMR of 237 in 2014-16(8). Telangana state went from an MMR of 92 in the 2011 to 2013 period to rate of 81 between 2014 and 2016(9).
Objectives:
1) To evaluate the causes of maternal deaths and risk factors associated with maternal mortality.
2) To determine the preventable factors in relation to maternal deaths.
Methodology:
This retrospective study was done at Prathima Institute of Medical Sciences, Nagunoor, Karimnagar, includes 24 cases of maternal deaths over a period of 10 years from Jan 2009 to Dec 2019. All booked or unbooked cases of maternal deaths that are admitted at the times of pregnancy, delivery, postpartum period were included in the study. The data was collected from hospital medical records. The medical records sheets of all identified women were received regarding age, parity, residence (rural or urban) antenatal booking states and cause of maternal death Permission of ethical committee of institute was obtained before recording data on proforma with the assurance of its confidentiality.
3) Delay in receiving adequate care once a woman arrives to medical facility.
In this study 87.5% mothers were from rural areas and 12.5% were from urban area. In contrast Jadhav et.al (10) in their study 64.55% were from urban residence and only 35.45% were from rural residence.
Majority of deaths occurred ante partum period (70.84%) compared to post partum period (29.16%). In contrast to Bhosale et al, in their study revealed 66.7% maternal deaths happened in the post partum period, followed by ante partum period (29.20%).
In our study majority of maternal deaths was observed in women of age group 20-25 years similarly Bangal et. al(11), In their study observed that 55.27% maternal death were in the age group of 19-24 years.
The study revealed that 58.4% maternal deaths were due to direct causes and 41.6% were due to indirect causes. Others studies have shown variations in direct obstetrical deaths, 68.70% in a study by Kulkarni et.al and 60% by Salhan et.al. Common direct causes of maternal mortality in our study were Eclampsia (20.8%), Sepsis (16.7%) and Hemorrhage (12.5%). In a study by Bangal et.al Haemorrhage (21.05%), Eclampsia and Pulmonary embolism (10.52%) and Sepsis (07.89%) were the main direct causes of maternal mortality. 40-60% of maternal deaths are considered preventable(12-15).
To increase access to quality maternal health services, India has doubled coverage of essential maternal health services leading to more institutional deliveries, which is almost tripled from 18% in 2005 to 52% in 2016.
India has introduced “Janani shishu suraksha karyakram” which allows all pregnant women delivering in public health institution to free transport and no expense delivery, including caesarean section has largely closed the urban or rural divide traditionally seen in institutional births. Campaigns such as “Pradhan MantrI Surakshit Matritva Abhiyan” have been introduced with great impact allowing women access to antenatal checkups, obstetric gynaecologists and to track high risk pregnancies, exactly what is need to make further gains and achieve the SDG targets.
To reduce maternal mortality telangana state introduced “Amma Vodi (Mother Lap)” programme under which 24 hour call centres were setup. The PHC’S worked with accredited social health activists (ASHAS) and collected the expected delivery dates of women in a particular locality and passed it on through the call centres. This allowed to screen high risk pregnancies and to make sure that all pregnant women are getting adequate care.
To prevent delay in the transport government introduced 102 Ambulance, incentive institutional deliveries and KCR KIT scheme were introduced to promote safe institutional deliveries.
CONCLUSION
Antenatel care with periodic measurements of blood pressure potentially prevents 70% of eclampsia by early detection of pre-eclampsia, use of anti hypertensives, magnesium sulphate and early termination will reduce deaths due to eclampsia. Observance of six cleans at the time of delivery and infection control practices(16) are to be strictly followed to reduce death due to sepsis.
Using oxytocin and misoprostol for prevention of postpartum haemorrhage, using timely blood transfusions, deaths due to haemorrhage can be reduced. Most deaths could have been prevented with help of early referral quick efficient transport facilities availability of blood and good intensive care support and by promoting overall safe motherhood.
REFERENCES:
1. Alkema L, chou D, Hogan D, et.al. Global, regional and national levels and trends in maternal mortality between 1990 and 2015, with scenario based projections to 2030. A systematic analysis by the UN maternal mortality estimation Inter-agency group Lancet 2016; 387:462
2. World health organization. Maternal mortality. https// www.who.int/news-room/fact-sheets/detail/maternalmortality.
3. GBD 2015 maternal mortality collaborators. Global, regional and national levels of maternal mortality, 1990- 2015: a systematic analysis for the global burden of disease study 2015. Lancet 2016; 388:1775.
4. UNICEF. Maternal and perinatal death enquiry and response empowering communities to avert maternal deaths in India (online) available at http//www.unicef.org/ india/mapdeir maternal-and-perinatal death-inquiry-andresponse- india.pdf.
5. Office of the Registrar general and census commissioner (India). India SRS special bulletin on maternal mortality 2007-2009. New Delhi, India:2011.
6. Office of the Registrar general and census commissioner, India. Special bulletin on maternal mortality in India 2010- 2012. Sample registration system.
http://www.censusindia.gov.in.
7. Dr.Poonam Khetrapal Singh, India has achieved ground breaking success in reducing maternal mortality.
http://www.searo.who.int/mediacentre/features/2018/ india-groundbreaking-success-reducing-maternalmortality- rate/en/.
8. Shoba Suri, An analysis of maternal health condition across parliamentary constituencies in india.http:// www.orfonline-org-cdn.ampproject.org.
9. Maternal morality rate in telangana drops to 81 inches closer to subtainable mark. https://m-timesofindiacom. cdn.ampproject.org.
10. Jadhav CA, Prabhakar G, Shinde MA, Tirankar VR, maternal mortality five year experience in tertiary care centre Indian J basic appl med res 2013;7(2):702-9.
11. Bangal VB, Giri PA, Garg R, maternal mortality at a tertiary care teaching hospital of rural india; a retrospective study Int J biol med res 2011; 2(4):1043-6.
12. Petersen EE, Davis NL , Good man D et.al, Vital signs pregnancy-related deaths. United states, 2001-2015 and strategies for prevention, 13 states, 2013-2017 MMWR Morb Mortal wkly Rep 2019;68:423.
13. Berg CJ,Harper MA, Atkinson SM et.al, preventability of pregnancy- related deaths; results of a state wide review obstetric,gynaecology 2005;106:1228.
14. Cantwell R, Clutton Brock T, Cooper G et.al, saving mothers lives receiving maternal deaths to make motherhood safer; 2006-2008, the eighth report of the confidential enquiries in to maternal deaths in the united kingdom.
15. Knight M, Mair M, Tuffnell D, Kenyon S, Shelenpeare J, Brock Lehurst P, Kurinczut JJ (EDS) saving lives improving mothers care surveillance of maternal deaths in the UK 2012-14.
16. Doddamani U, Rampur N, Kaveri, Pooja, A study of maternal mortality in a tertiary care hospital. Int J reprod contracept obstet gynaecology 2018;7:2446-8.
How to cite this article : Satyaprabha S, Vivekananda A, Mythreai, Wilson V. A Retrospective Study On Maternal Deaths And Its Causes In A Tertiary Care Teaching Institute In Northern Telangana. Perspectives in Medical Research 2019; 7(2):71-74
Sources of Support: Nil,Conflict of interest:None declared
Year : 2019 | Volume : 7 | Issue : 2 Page : 71-74
Satyaprabha S1, Vivekananda A2, Mythreai3, Wilson V4
1DEPARTMENT OF OBG, 2DEPARTMENT OF COMMUNITY MEDICINE.
*Address for correspondence:: Department of OBG , Prathima Institute of Medical Sciences,Nagnur road, Karimnagar 505001
Background:
Maternal mortality is a strong indicator for measuring the health care provided to the women by any society. Although pregnancy is considered physiological at times it leads to morbidity and even death. The aim of the study is to evaluate various epidemiological factors, causes of maternal mortality and to determine the preventable factors associated with maternal deaths.
Method:
A retrospective hospital based study was conducted in the Department of OBG, Prathima Institute of Medical Sciences, A tertiary care hospital in Karimnagar, Telangana State, India, over a period of 10 years from Jan 2009 to Dec 2018.
Results:
A total of 24 deaths were analysed. Maximum number of deaths were seen in age group 20-24 years, More deaths were seen in ante partum period (70.84%) than post partum period (29.16%). Most of them were unbooked (87.5%). than booked cases (12.5%). The classic triad of hypertensive disorders (20.8%) Sepsis (16.7%) and Haemorrhage (12.5%) were the major direct causes. Hepatitis, Heart disease in pregnancy, Respiratory disease are the common indirect causes.
Conclusion:
Majority of deaths were preventable by proper antenatal care, early detection of high risk pregnancies and timely referral to higher centre.
Keywords: Maternal mortality, Eclampsia, Haemorrhage, Sepsis, Maternal mortality ratio.
INTRODUCTION Globally maternal mortality has been falling with substantial variation among countries and within countries (1,2). The MMR was 216 maternal deaths/ 1Lakh live births in 2015 globally (1, 2, 3).country specific MMR estimates ranged from 3 (Finland) to 1360 (Sierra leone) maternal deaths/1Lakh live births.
The need for continued efforts to eliminate preventable maternal deaths is highlighted by the gap between the sustainable development goal of fewer than 70 maternal deaths/1Lakh live births globally by 2030, and recent MMR of low performing regions, which is nearly 20 times the goal MMR.
Maternal death can be defined as the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of pregnancy, from any cause related to aggravated by the pregnancy or its management but not from accidental or incidental causes.(4) A direct obstetric death results from obstetric complications of pregnancy, delivery or the post partum period and from interventions, omissions, incorrect treatment or a chain of events related to the obstetric complication (3) An indirect obstetric death results from pre-existing disease (Eg: diabetis, cardiac disease, malaria, tuberculosis, HIV) or new disease that develops during pregnancy and is unrelated to pregnancy but is aggravated by the physiologic effects of pregnancy (Eg: Influenza) India has ground breaking progress in recent years in reducing MMR by 77% from 556 per 1lakh live births in 1990 to 130 per 1lakh live births in 2016 (5, 7) India’s present MMR is below the millennium development goal (MDG) (6) target and puts the country on track to achieve the sustainable development goal (SDG). Kerala has MMR of 46, while Assam has MMR of 237 in 2014-16(8). Telangana state went from an MMR of 92 in the 2011 to 2013 period to rate of 81 between 2014 and 2016(9).
Objectives:
1) To evaluate the causes of maternal deaths and risk factors associated with maternal mortality.
2) To determine the preventable factors in relation to maternal deaths.
Methodology:
This retrospective study was done at Prathima Institute of Medical Sciences, Nagunoor, Karimnagar, includes 24 cases of maternal deaths over a period of 10 years from Jan 2009 to Dec 2019. All booked or unbooked cases of maternal deaths that are admitted at the times of pregnancy, delivery, postpartum period were included in the study. The data was collected from hospital medical records. The medical records sheets of all identified women were received regarding age, parity, residence (rural or urban) antenatal booking states and cause of maternal death Permission of ethical committee of institute was obtained before recording data on proforma with the assurance of its confidentiality.
3) Delay in receiving adequate care once a woman arrives to medical facility.
In this study 87.5% mothers were from rural areas and 12.5% were from urban area. In contrast Jadhav et.al (10) in their study 64.55% were from urban residence and only 35.45% were from rural residence.
Majority of deaths occurred ante partum period (70.84%) compared to post partum period (29.16%). In contrast to Bhosale et al, in their study revealed 66.7% maternal deaths happened in the post partum period, followed by ante partum period (29.20%).
In our study majority of maternal deaths was observed in women of age group 20-25 years similarly Bangal et. al(11), In their study observed that 55.27% maternal death were in the age group of 19-24 years.
The study revealed that 58.4% maternal deaths were due to direct causes and 41.6% were due to indirect causes. Others studies have shown variations in direct obstetrical deaths, 68.70% in a study by Kulkarni et.al and 60% by Salhan et.al. Common direct causes of maternal mortality in our study were Eclampsia (20.8%), Sepsis (16.7%) and Hemorrhage (12.5%). In a study by Bangal et.al Haemorrhage (21.05%), Eclampsia and Pulmonary embolism (10.52%) and Sepsis (07.89%) were the main direct causes of maternal mortality. 40-60% of maternal deaths are considered preventable(12-15).
To increase access to quality maternal health services, India has doubled coverage of essential maternal health services leading to more institutional deliveries, which is almost tripled from 18% in 2005 to 52% in 2016.
India has introduced “Janani shishu suraksha karyakram” which allows all pregnant women delivering in public health institution to free transport and no expense delivery, including caesarean section has largely closed the urban or rural divide traditionally seen in institutional births. Campaigns such as “Pradhan MantrI Surakshit Matritva Abhiyan” have been introduced with great impact allowing women access to antenatal checkups, obstetric gynaecologists and to track high risk pregnancies, exactly what is need to make further gains and achieve the SDG targets.
To reduce maternal mortality telangana state introduced “Amma Vodi (Mother Lap)” programme under which 24 hour call centres were setup. The PHC’S worked with accredited social health activists (ASHAS) and collected the expected delivery dates of women in a particular locality and passed it on through the call centres. This allowed to screen high risk pregnancies and to make sure that all pregnant women are getting adequate care.
To prevent delay in the transport government introduced 102 Ambulance, incentive institutional deliveries and KCR KIT scheme were introduced to promote safe institutional deliveries.
CONCLUSION
Antenatel care with periodic measurements of blood pressure potentially prevents 70% of eclampsia by early detection of pre-eclampsia, use of anti hypertensives, magnesium sulphate and early termination will reduce deaths due to eclampsia. Observance of six cleans at the time of delivery and infection control practices(16) are to be strictly followed to reduce death due to sepsis.
Using oxytocin and misoprostol for prevention of postpartum haemorrhage, using timely blood transfusions, deaths due to haemorrhage can be reduced. Most deaths could have been prevented with help of early referral quick efficient transport facilities availability of blood and good intensive care support and by promoting overall safe motherhood.
REFERENCES:
1. Alkema L, chou D, Hogan D, et.al. Global, regional and national levels and trends in maternal mortality between 1990 and 2015, with scenario based projections to 2030. A systematic analysis by the UN maternal mortality estimation Inter-agency group Lancet 2016; 387:462
2. World health organization. Maternal mortality. https// www.who.int/news-room/fact-sheets/detail/maternalmortality.
3. GBD 2015 maternal mortality collaborators. Global, regional and national levels of maternal mortality, 1990- 2015: a systematic analysis for the global burden of disease study 2015. Lancet 2016; 388:1775.
4. UNICEF. Maternal and perinatal death enquiry and response empowering communities to avert maternal deaths in India (online) available at http//www.unicef.org/ india/mapdeir maternal-and-perinatal death-inquiry-andresponse- india.pdf.
5. Office of the Registrar general and census commissioner (India). India SRS special bulletin on maternal mortality 2007-2009. New Delhi, India:2011.
6. Office of the Registrar general and census commissioner, India. Special bulletin on maternal mortality in India 2010- 2012. Sample registration system.
http://www.censusindia.gov.in.
7. Dr.Poonam Khetrapal Singh, India has achieved ground breaking success in reducing maternal mortality.
http://www.searo.who.int/mediacentre/features/2018/ india-groundbreaking-success-reducing-maternalmortality- rate/en/.
8. Shoba Suri, An analysis of maternal health condition across parliamentary constituencies in india.http:// www.orfonline-org-cdn.ampproject.org.
9. Maternal morality rate in telangana drops to 81 inches closer to subtainable mark. https://m-timesofindiacom. cdn.ampproject.org.
10. Jadhav CA, Prabhakar G, Shinde MA, Tirankar VR, maternal mortality five year experience in tertiary care centre Indian J basic appl med res 2013;7(2):702-9.
11. Bangal VB, Giri PA, Garg R, maternal mortality at a tertiary care teaching hospital of rural india; a retrospective study Int J biol med res 2011; 2(4):1043-6.
12. Petersen EE, Davis NL , Good man D et.al, Vital signs pregnancy-related deaths. United states, 2001-2015 and strategies for prevention, 13 states, 2013-2017 MMWR Morb Mortal wkly Rep 2019;68:423.
13. Berg CJ,Harper MA, Atkinson SM et.al, preventability of pregnancy- related deaths; results of a state wide review obstetric,gynaecology 2005;106:1228.
14. Cantwell R, Clutton Brock T, Cooper G et.al, saving mothers lives receiving maternal deaths to make motherhood safer; 2006-2008, the eighth report of the confidential enquiries in to maternal deaths in the united kingdom.
15. Knight M, Mair M, Tuffnell D, Kenyon S, Shelenpeare J, Brock Lehurst P, Kurinczut JJ (EDS) saving lives improving mothers care surveillance of maternal deaths in the UK 2012-14.
16. Doddamani U, Rampur N, Kaveri, Pooja, A study of maternal mortality in a tertiary care hospital. Int J reprod contracept obstet gynaecology 2018;7:2446-8.
How to cite this article : Satyaprabha S, Vivekananda A, Mythreai, Wilson V. A Retrospective Study On Maternal Deaths And Its Causes In A Tertiary Care Teaching Institute In Northern Telangana. Perspectives in Medical Research 2019; 7(2):71-74
Sources of Support: Nil,Conflict of interest:None declared
Open Access
Perspectives in Medical Research is committed to keeping research articles Open Access.Journal permits any users to read, download, copy, print, search, or link to the full texts of these articles...
Read more
© PIMR.org.in - 2013. All Rights Reserved.
