
advertise here
Original Article
The study of anatomy of main pancreatic duct and its variations.
Year : 2019 | Volume : 7 | Issue : 2 Page : 31-37
Introduction:
The duct system of pancreas consists of two large ducts – Main pancreatic duct and Accessory pancreatic duct. Both these ducts drain the entire exocrine part of pancreas. Main pancreatic duct is always present while accessory pancreatic duct may be absent in 30% cases. The study of duct system of pancreas has wide application in pancreatitis, endoscopic retrograde cholangiopancreaticogram, pancreatic calculi, carcinoma of pancreas and even in obstructive jaundice caused by gall stone disease and also in gall bladder carcinoma. Materials & Methods: The present study was done in 50 adult formalin fixed pancreatic specimens removed during posterior abdominal wall dissection. Statistical analysis: Done using Mean, Standard deviation, Percentage
Results:
The study showed that the mean length and standard deviation of the main pancreatic duct was 18.4 ± 2.43 cm and the mean width and standard deviation of the duct was 2.7 ± 0.8 mm, 2.3 ± 0.5 mm 2.1 ± 0.2 mm respectively in the head, body and the tail. The main pancreatic duct coursed from tail to its opening into the duodenum through five various types Descending (46%), Vertical (4%), Loop(2%) , Sigmoid(30%) and Horizontal(18%). The main pancreatic duct opened into the major duodenal papillae in 72% specimens. Conclusion: The mean length of the main pancreatic duct varies from 13.4 to 26.cm, while the width of the duct gradually increases from tail to head. Descending type was most common while loop type was least common type of the main pancreatic duct course. The main drainage route of the pancreas was through major duodenal papilla. Keywords: Main pancreatic duct, Length, Width, Type, Drainage route
INTRODUCTION
Pancreas is a mixed exocrine and endocrine gland. The exocrine part of the gland is drained by main and accessory pancreatic ducts. The main pancreatic duct begins in the tail of the pancreas by union of interlobular ducts, courses through the body and neck where it curves downwards, backwards and opens into the duodenum through major duodenal papilla after the formation of hepato-pancreatic ampulla by uniting with common bile duct.
The distal part of the main pancreatic duct is formed from the embryonic dorsal pancreatic duct while the proximal part of the duct is formed from the embryonic ventral pancreatic duct and also from the communication formed between the ventral and dorsal pancreatic ducts during the process of development. Thus the main pancreatic duct undergoes variations in size, course and its opening into the duodenal papillae. The non-union of the embryological ducts results in the persistence of the dorsal and ventral ducts which is called pancreas divisum / embryonic type of duct system. The knowledge of these variations in the duct system of pancreas is very important clinically and surgically. Ductal length is the main factor influencing the choice of the surgical procedures like pancreatico-jujunostomy or pancreatic resection and its study helps in differentiating the congenital anomalies like partial agenesis of pancreas. The study of width has clinical significance in pancreatitis and pancreatic cancer/ malignancy. The knowledge of course and opening of the main pancreatic duct is essential in the management of the acute or chronic pancreatitis, in endoscopic retrograde cholangiopancreaticography and also in cholelithiasis and gall bladder carcinoma.
MATERIALS AND METHODS
The study was done in 50 adult formalin fixed specimens of pancreas and duodenum en-bloc obtained during dissection of posterior abdominal wall. The study was made regardless of age and sex.
The duct system was approached from the posterior surface of the pancreas by piecemeal dissection of the substance of the gland. The main pancreatic duct was identified first in the body of the pancreas and later it was traced to both ends i.e., tail and duodenal wall. The common bile duct and the hepato-pancreatic ampulla were exposed. The length of the ducts was measured using a thread and a manual vernier calipers.
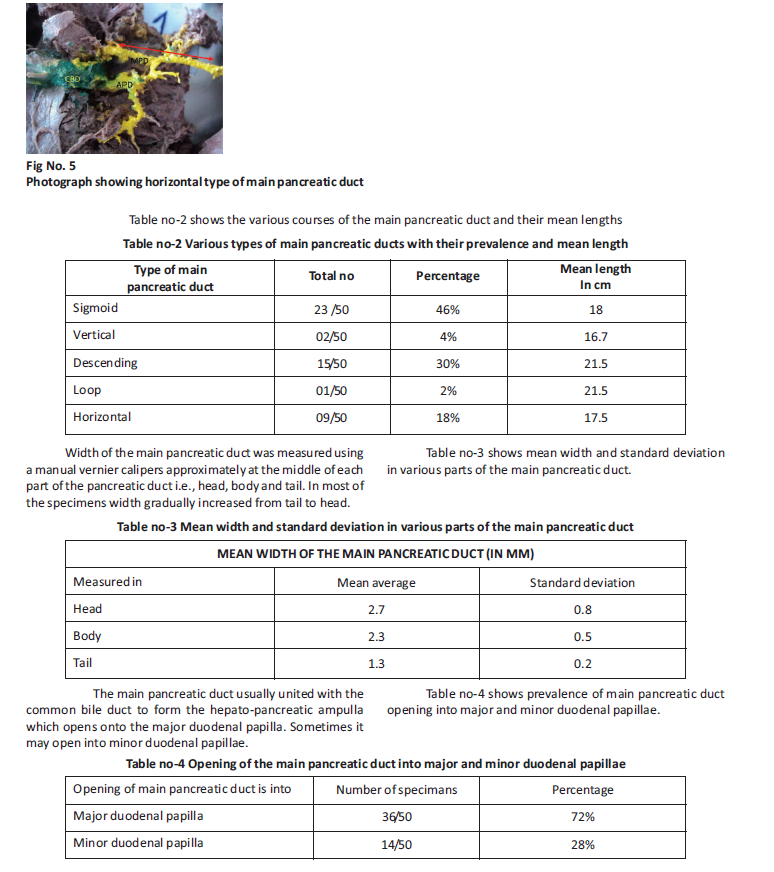
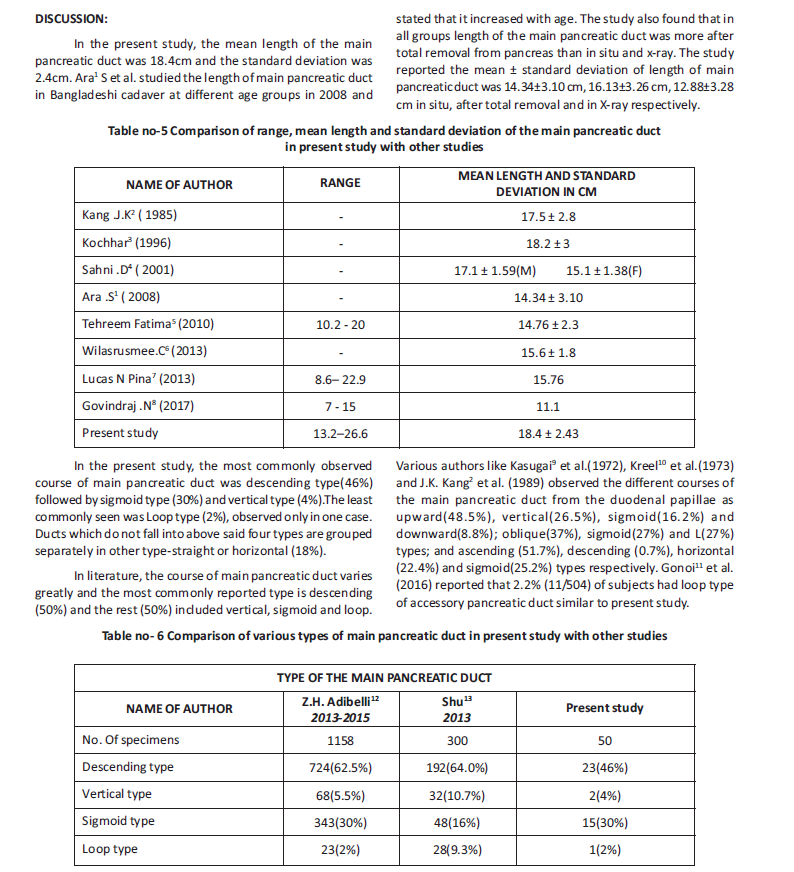
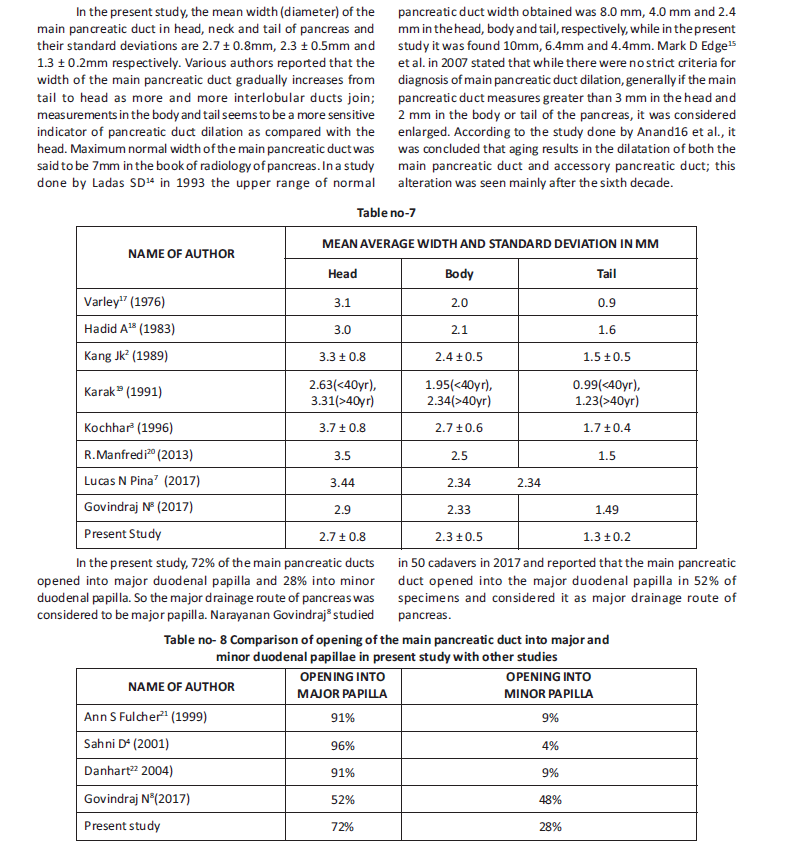
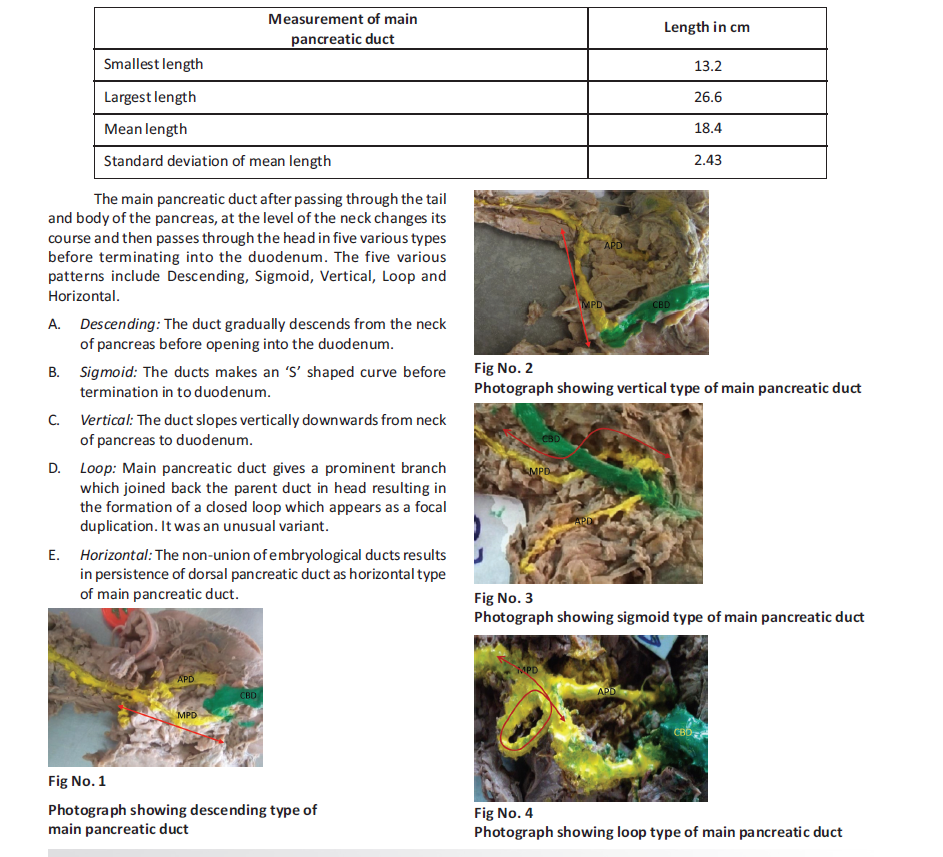
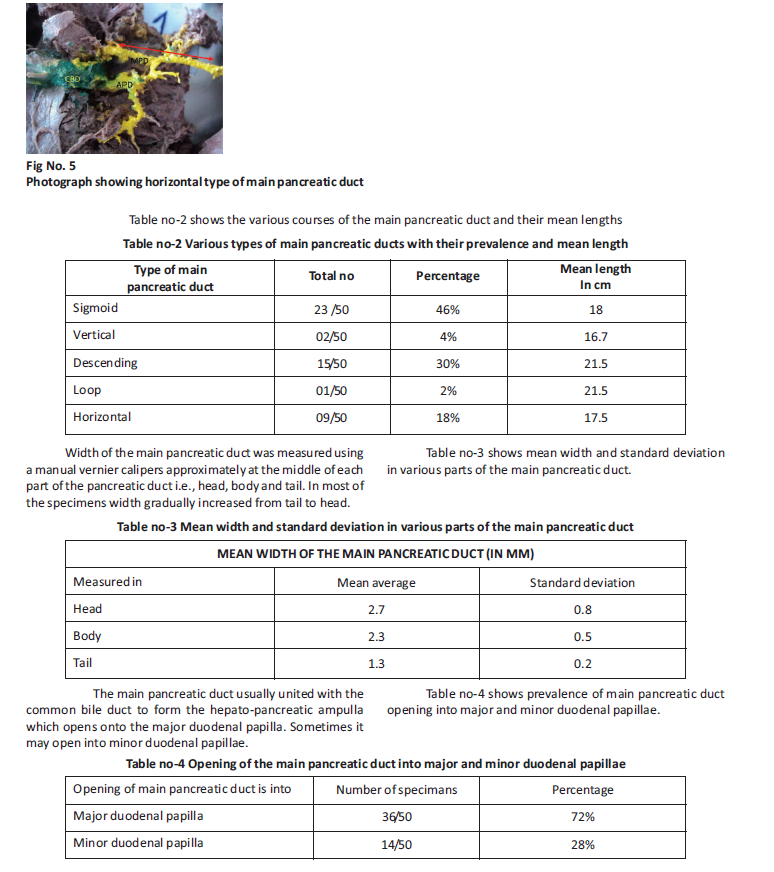
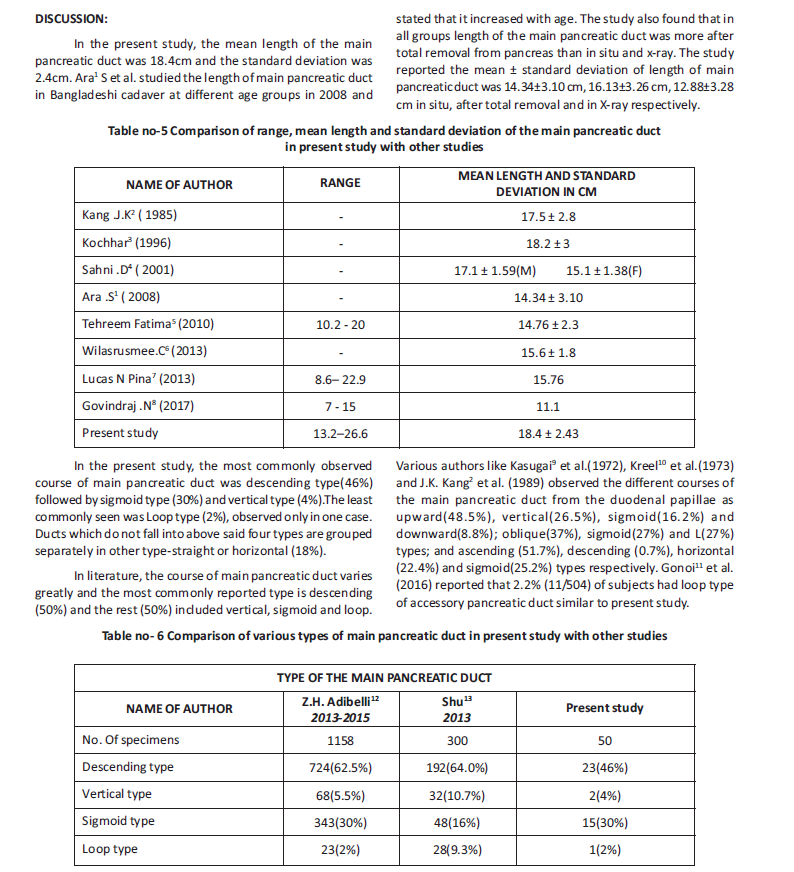
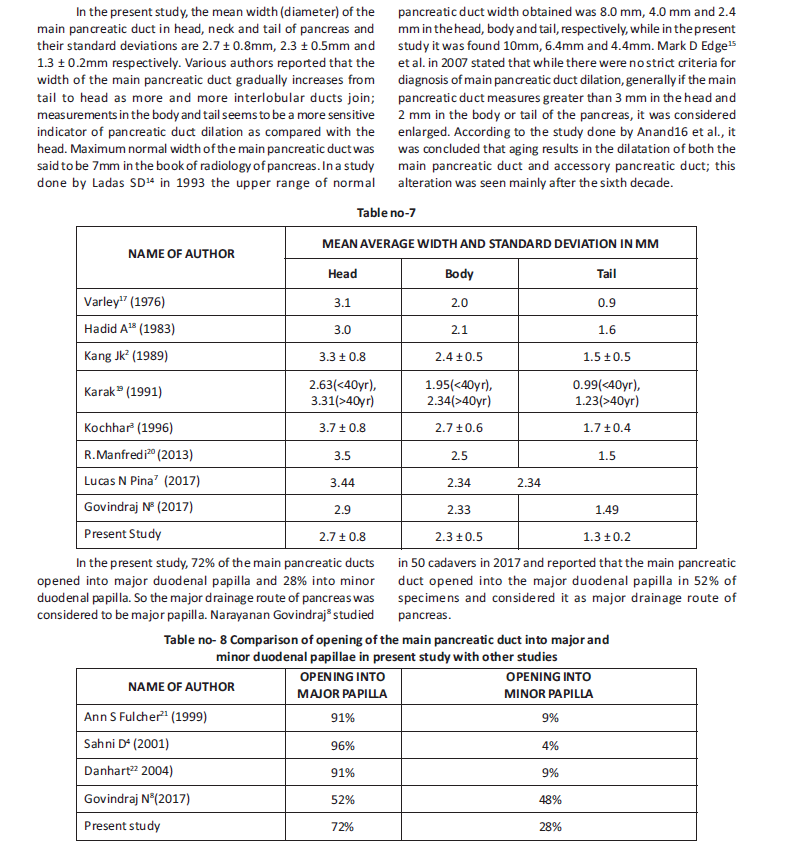
The duodenum was opened on the right side and the estimated entrance point for the pancreatic duct and common bile duct into the duodenal lumen was made. The entire duct system was colored using different paints and photographs of the patterns were taken.
RESULTS
The main pancreatic duct was measured from its formation by the union of the interlobular ducts in the tail of pancreas to its termination either by uniting with common bile duct or its direct opening into the duodenum. Table no-1 shows the various measurements of the main pancreatic duct. Table no-1 Mean length and standard deviation of the main pancreatic duct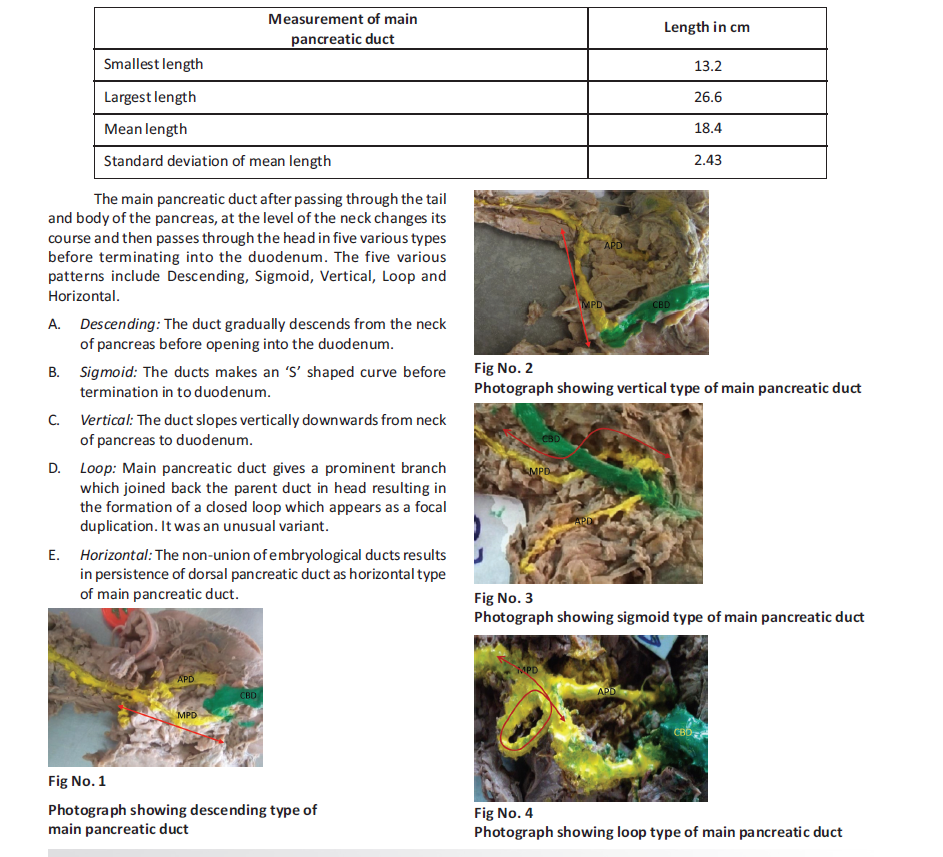
CONCLUSION:
The mean length of the main pancreatic duct varies from 13.4 to 26.cm.
The mean width of the duct gradually increases from tail to head with the mean width being 1.3mm, 2.3mm and 2.7mm respectively in the tail, body and head of pancreas. The type/course of the main pancreatic duct depends on the method of development of the communication between main and accessory pancreatic ducts. Descending type was the most common while loop type was the least common type. The prevalence of vertical and sigmoid course was markedly different which may be because of ethnicity. Horizontal type was the persistent embryonic dorsal pancreatic duct.
The main drainage route of the pancreas is through major duodenal papilla. The opening of main pancreatic duct into minor duodenal papilla may be due to non union of pancreatic ducts, after fusion of dorsal and ventral pancreas during development. This type of drainage pattern here was associated with development of communication between the main and the accessory pancreatic duct to reduce load on the minor papilla while diverting some of its contents into duodenum through major papilla; or it was not involved in the formation of hepato-pancreatic ampulla thus preventing the load of common bile duct on the smaller minor papilla.
REFERENCES:
1. S Ara, Shahriah S, Begum S. The length of main pancreatic duct in Bangladeshi cadaver at different age groups. Mymensingh Med J. 2011 Apr;20(2):298-30.
2. Kang JK, Chung JB, Moon YM, Choi HJ. The normal endoscopic pancreatogram in Koreans. Korean Journal of Internal Medicine. (1989).
3. Kochhar. Narayanan govindraj, shabna. C. Variations in the duct system of pancreas: A cadaveric study. Int j anat res 2017;5(3.1):4136-4143. Doi: 10.16965/ijar.2017.269.
4. Sahni D, Jit I, Harjeet. Gross anatomy of the pancreatic ducts in north Indians . Trop Gastroenterol. 2001 Oct- Dec;22 (4):197-201.
5. Tehreem Fatima. Anatomical Variants of Pancreatic Duct System In Human Cadavers, jfjmc, vol.4, jul – sept 2010.
6. Wilasrusmee.C, Pongchairerks P. Pancreaticobiliary ductal anatomy in Thai people. J Hepatobiliary Pancreat Surg. 1999;6(1):79-85.
7. Lucas .N. Pina, Does the Accessory Pancreatic Duct have any Protective Role in Acute Biliary Pancreatitis? Anatomical Findings from Cadaver Dissections , MOJ Anat & Physiol 2016, 2(7): 00071.
8. Narayanan Govindraj, Shabna.C 2. Variations in the duct system of pancreas: a cadaveric study International Journal of Anatomy and Research, Int J Anat Res 2017, Vol 5(3.1):4136-43. ISSN 2321-4287.
9. Kasugai T, Kuno N, Nobayashi S. Endoscopic pancreatocholangiography. I. The normal endoscopic pancreatocholangiogram. Gastroenterology 63:217. 1972; 10. Kreel L, Sandin B, Slavin G. Pancreatic morphology. A combined radiological and pathological study. Clin Radiol 24:154. 1973;
11. Gonoi. Akai H, Hagiwara K, Akahane M, Hayashi N, et al. (2011) Pancreas divisum as a predisposing factor for chronic and recurrent idiopathic pancreatitis: initial in vivo survey. Gut 60: 1103–1108.W.
12. Zehra Hilal Adebilli, Anatomic variations of the pancreatic duct and their relevance with the Cambridge classification system: MRCP findings of 1158 consecutive patients . Radiol Oncol 2016; 50(4): 370-377.
13. Shu.J, Zhang XM, Zhao JN, Zeng NL Normal pancreatic duct: Evaluation with MR cholangiopancreatography .Chinese Journal of Medical Imaging Technology 2006; 22(4):584-7 .
14. Ladas SD. Tassios PS, Giorgiotis K, Rokkas T, Theodosiou P, Raptis SA Pancreatic duct width: its significance as a diagnostic criterion for pancreatic disease. Hepatogastroenterology. 1993 Feb;40(1):52-5.
15. Mark D Edge. Edge MD, Hoteit M, Patel AP, Wang X, Baumgarten DA, Cai Q. Clinical significance of main pancreatic duct dilation on computed tomography: Single and double duct dilation. World Journal of Gastroenterology : WJG. 2007;1 3(11):1701-1705. doi:10.3748/wjg.v13.i11.1701.
16. S Anand Rani. ,Sumathi Latha,Patency of accessory pancreatic duct and its relation with duodenal inter papillary distance, S. Indian J Gastroenterol (2012) 31: 24. https://doi.org/10.1007/s12664-011-0150.
17. Varley PF, Rohrmann CA Jr, Silvis SE, Vennes JA .The normal endoscopic pancreatogram. Radiology. 1976 Feb;118 (2):295-300.
18. Hadid A. Pancreatic duct diameter: sonographic measurement in normal subjects. J Clin Ultrasound. 1983 Jan;11(1):17-22
19. Karak PK, Vashisht S, Tandon RK, Berry MNormal endoscopic pancreatogram in an Indian referral hospital. Indian J Med Res. 1991 Dec;94:426-9.
20. Manfredi. Magnetic Resonance Cholangiopan creatography (MRCP): Biliary and Pancreatic Ducts.
Riccardo Manfredi, Roberto Pozzi Mucelli.2013.Pg 20-30 21. Ann.s.fulcher. Turner MA, Capps GW, Zfass AM, Baker KM, Half-Fourier RARE MRCP in 300 subjects. Radiology 1998; 207: 21-32.
22. Dahnert. Oxford handbook of Medical Imaging, 7th Edition, Michael J Darby, Dominic A Barron, Rachel E Hyland, 2012, Pg:341-357.
How to cite this article : Malathi K , Kishan Reddy C. The study of anatomy of main pancreatic duct and its variations. Perspectives in Medical Research 2019; 7(2):31-37
Sources of Support: Nil,Conflict of interest:None declared
Year : 2019 | Volume : 7 | Issue : 2 Page : 31-37
Author: - Dr Malathi K1, Dr Kishan Reddy C2
1Associate professor, 2Professor & HOD, Department of Anatomy, , Prathima Institute of Medical Sciences,
Nagunoor, Karimnagar, Telangana, India..
*Address for correspondence:: Dr K Malathi, Assistant Professor, Department of Anatomy, Prathima Institute of Medical
Sciences, Nagunoor , Karimnagar, Telangana, India.
E mail ID: - [email protected]
Introduction:
The duct system of pancreas consists of two large ducts – Main pancreatic duct and Accessory pancreatic duct. Both these ducts drain the entire exocrine part of pancreas. Main pancreatic duct is always present while accessory pancreatic duct may be absent in 30% cases. The study of duct system of pancreas has wide application in pancreatitis, endoscopic retrograde cholangiopancreaticogram, pancreatic calculi, carcinoma of pancreas and even in obstructive jaundice caused by gall stone disease and also in gall bladder carcinoma. Materials & Methods: The present study was done in 50 adult formalin fixed pancreatic specimens removed during posterior abdominal wall dissection. Statistical analysis: Done using Mean, Standard deviation, Percentage
Results:
The study showed that the mean length and standard deviation of the main pancreatic duct was 18.4 ± 2.43 cm and the mean width and standard deviation of the duct was 2.7 ± 0.8 mm, 2.3 ± 0.5 mm 2.1 ± 0.2 mm respectively in the head, body and the tail. The main pancreatic duct coursed from tail to its opening into the duodenum through five various types Descending (46%), Vertical (4%), Loop(2%) , Sigmoid(30%) and Horizontal(18%). The main pancreatic duct opened into the major duodenal papillae in 72% specimens. Conclusion: The mean length of the main pancreatic duct varies from 13.4 to 26.cm, while the width of the duct gradually increases from tail to head. Descending type was most common while loop type was least common type of the main pancreatic duct course. The main drainage route of the pancreas was through major duodenal papilla. Keywords: Main pancreatic duct, Length, Width, Type, Drainage route
INTRODUCTION
Pancreas is a mixed exocrine and endocrine gland. The exocrine part of the gland is drained by main and accessory pancreatic ducts. The main pancreatic duct begins in the tail of the pancreas by union of interlobular ducts, courses through the body and neck where it curves downwards, backwards and opens into the duodenum through major duodenal papilla after the formation of hepato-pancreatic ampulla by uniting with common bile duct.
The distal part of the main pancreatic duct is formed from the embryonic dorsal pancreatic duct while the proximal part of the duct is formed from the embryonic ventral pancreatic duct and also from the communication formed between the ventral and dorsal pancreatic ducts during the process of development. Thus the main pancreatic duct undergoes variations in size, course and its opening into the duodenal papillae. The non-union of the embryological ducts results in the persistence of the dorsal and ventral ducts which is called pancreas divisum / embryonic type of duct system. The knowledge of these variations in the duct system of pancreas is very important clinically and surgically. Ductal length is the main factor influencing the choice of the surgical procedures like pancreatico-jujunostomy or pancreatic resection and its study helps in differentiating the congenital anomalies like partial agenesis of pancreas. The study of width has clinical significance in pancreatitis and pancreatic cancer/ malignancy. The knowledge of course and opening of the main pancreatic duct is essential in the management of the acute or chronic pancreatitis, in endoscopic retrograde cholangiopancreaticography and also in cholelithiasis and gall bladder carcinoma.
MATERIALS AND METHODS
The study was done in 50 adult formalin fixed specimens of pancreas and duodenum en-bloc obtained during dissection of posterior abdominal wall. The study was made regardless of age and sex.
The duct system was approached from the posterior surface of the pancreas by piecemeal dissection of the substance of the gland. The main pancreatic duct was identified first in the body of the pancreas and later it was traced to both ends i.e., tail and duodenal wall. The common bile duct and the hepato-pancreatic ampulla were exposed. The length of the ducts was measured using a thread and a manual vernier calipers.
The duodenum was opened on the right side and the estimated entrance point for the pancreatic duct and common bile duct into the duodenal lumen was made. The entire duct system was colored using different paints and photographs of the patterns were taken.
RESULTS
The main pancreatic duct was measured from its formation by the union of the interlobular ducts in the tail of pancreas to its termination either by uniting with common bile duct or its direct opening into the duodenum. Table no-1 shows the various measurements of the main pancreatic duct. Table no-1 Mean length and standard deviation of the main pancreatic duct
CONCLUSION:
The mean length of the main pancreatic duct varies from 13.4 to 26.cm.
The mean width of the duct gradually increases from tail to head with the mean width being 1.3mm, 2.3mm and 2.7mm respectively in the tail, body and head of pancreas. The type/course of the main pancreatic duct depends on the method of development of the communication between main and accessory pancreatic ducts. Descending type was the most common while loop type was the least common type. The prevalence of vertical and sigmoid course was markedly different which may be because of ethnicity. Horizontal type was the persistent embryonic dorsal pancreatic duct.
The main drainage route of the pancreas is through major duodenal papilla. The opening of main pancreatic duct into minor duodenal papilla may be due to non union of pancreatic ducts, after fusion of dorsal and ventral pancreas during development. This type of drainage pattern here was associated with development of communication between the main and the accessory pancreatic duct to reduce load on the minor papilla while diverting some of its contents into duodenum through major papilla; or it was not involved in the formation of hepato-pancreatic ampulla thus preventing the load of common bile duct on the smaller minor papilla.
REFERENCES:
1. S Ara, Shahriah S, Begum S. The length of main pancreatic duct in Bangladeshi cadaver at different age groups. Mymensingh Med J. 2011 Apr;20(2):298-30.
2. Kang JK, Chung JB, Moon YM, Choi HJ. The normal endoscopic pancreatogram in Koreans. Korean Journal of Internal Medicine. (1989).
3. Kochhar. Narayanan govindraj, shabna. C. Variations in the duct system of pancreas: A cadaveric study. Int j anat res 2017;5(3.1):4136-4143. Doi: 10.16965/ijar.2017.269.
4. Sahni D, Jit I, Harjeet. Gross anatomy of the pancreatic ducts in north Indians . Trop Gastroenterol. 2001 Oct- Dec;22 (4):197-201.
5. Tehreem Fatima. Anatomical Variants of Pancreatic Duct System In Human Cadavers, jfjmc, vol.4, jul – sept 2010.
6. Wilasrusmee.C, Pongchairerks P. Pancreaticobiliary ductal anatomy in Thai people. J Hepatobiliary Pancreat Surg. 1999;6(1):79-85.
7. Lucas .N. Pina, Does the Accessory Pancreatic Duct have any Protective Role in Acute Biliary Pancreatitis? Anatomical Findings from Cadaver Dissections , MOJ Anat & Physiol 2016, 2(7): 00071.
8. Narayanan Govindraj, Shabna.C 2. Variations in the duct system of pancreas: a cadaveric study International Journal of Anatomy and Research, Int J Anat Res 2017, Vol 5(3.1):4136-43. ISSN 2321-4287.
9. Kasugai T, Kuno N, Nobayashi S. Endoscopic pancreatocholangiography. I. The normal endoscopic pancreatocholangiogram. Gastroenterology 63:217. 1972; 10. Kreel L, Sandin B, Slavin G. Pancreatic morphology. A combined radiological and pathological study. Clin Radiol 24:154. 1973;
11. Gonoi. Akai H, Hagiwara K, Akahane M, Hayashi N, et al. (2011) Pancreas divisum as a predisposing factor for chronic and recurrent idiopathic pancreatitis: initial in vivo survey. Gut 60: 1103–1108.W.
12. Zehra Hilal Adebilli, Anatomic variations of the pancreatic duct and their relevance with the Cambridge classification system: MRCP findings of 1158 consecutive patients . Radiol Oncol 2016; 50(4): 370-377.
13. Shu.J, Zhang XM, Zhao JN, Zeng NL Normal pancreatic duct: Evaluation with MR cholangiopancreatography .Chinese Journal of Medical Imaging Technology 2006; 22(4):584-7 .
14. Ladas SD. Tassios PS, Giorgiotis K, Rokkas T, Theodosiou P, Raptis SA Pancreatic duct width: its significance as a diagnostic criterion for pancreatic disease. Hepatogastroenterology. 1993 Feb;40(1):52-5.
15. Mark D Edge. Edge MD, Hoteit M, Patel AP, Wang X, Baumgarten DA, Cai Q. Clinical significance of main pancreatic duct dilation on computed tomography: Single and double duct dilation. World Journal of Gastroenterology : WJG. 2007;1 3(11):1701-1705. doi:10.3748/wjg.v13.i11.1701.
16. S Anand Rani. ,Sumathi Latha,Patency of accessory pancreatic duct and its relation with duodenal inter papillary distance, S. Indian J Gastroenterol (2012) 31: 24. https://doi.org/10.1007/s12664-011-0150.
17. Varley PF, Rohrmann CA Jr, Silvis SE, Vennes JA .The normal endoscopic pancreatogram. Radiology. 1976 Feb;118 (2):295-300.
18. Hadid A. Pancreatic duct diameter: sonographic measurement in normal subjects. J Clin Ultrasound. 1983 Jan;11(1):17-22
19. Karak PK, Vashisht S, Tandon RK, Berry MNormal endoscopic pancreatogram in an Indian referral hospital. Indian J Med Res. 1991 Dec;94:426-9.
20. Manfredi. Magnetic Resonance Cholangiopan creatography (MRCP): Biliary and Pancreatic Ducts.
Riccardo Manfredi, Roberto Pozzi Mucelli.2013.Pg 20-30 21. Ann.s.fulcher. Turner MA, Capps GW, Zfass AM, Baker KM, Half-Fourier RARE MRCP in 300 subjects. Radiology 1998; 207: 21-32.
22. Dahnert. Oxford handbook of Medical Imaging, 7th Edition, Michael J Darby, Dominic A Barron, Rachel E Hyland, 2012, Pg:341-357.
How to cite this article : Malathi K , Kishan Reddy C. The study of anatomy of main pancreatic duct and its variations. Perspectives in Medical Research 2019; 7(2):31-37
Sources of Support: Nil,Conflict of interest:None declared
Open Access
Perspectives in Medical Research is committed to keeping research articles Open Access.Journal permits any users to read, download, copy, print, search, or link to the full texts of these articles...
Read more
© PIMR.org.in - 2013. All Rights Reserved.
