
advertise here
Original Article
Efficacy of optic nerve sheath diameter by ultrasound as a non-invasive
method to determine elevated intracranial pressure in Indian population.
Year : 2019 | Volume : 7 | Issue : 2 Page : 38-42
Introduction:
It is important to assess use of Optic Nerve sheath Diameter (ONSD) measurement by point of care ultrasonography (POCUS) as a non-invasive method for detecting elevated Intracranial Pressure (ICP) and to compare with Brain Computed Tomography (CT) findings of Elevated ICP in Indian population Methods:
This study was a Prospective Observational Study done in emergency Department of a tertiary care hospital in western India .Adult patients within 18-60 years age group, with Head trauma presenting with headache, vomiting, convulsions, loss of consciousness, and altered sensorium were included in the study.Non-trauma patients with focal neurological changes and history suggestive of possible spontaneous intracranial hemorrhage were also included. Data was recorded after stabilizing patients as per standard trauma and non-trauma protocol.
Patients underwent a POCUS study to measure the ONSD. Based on clinical judgment and ONSD measurement above the expected cut-off range, medical management for Elevated ICP was started. A Plain Brain CT Scan was obtained. Definitive treatment was planned after confirming on CT scan. ONSD measurement more than 6mm was suggestive of Elevated ICP Results:
108 patients were studied. A normal range of ONSD found was 3.5mm – 5.4mm.
26 patients had CT results consistent with Elevated ICP. All cases of CT-determined Elevated ICP were correctly predicted by ONSD. The sensitivity and specificity of this study is 98.75 % and 92.86% respectively.
Conclusion:
POCUS has the advantages of cost, time effective, non-invasive and reproducibility. It can be used as an additional diagnostic tool.
Keywords:
Optic nerve sheath diameter, Point of care Ultrasound, Intracranial pressure INTRODUCTION
Traumatic Brain Injury (TBI) is defined as impairment in brain function as a result of mechanical force. The dysfunction can be temporary or permanent, and may or may not result in underlying structural changes in the brain. [1] Any changes to the volume of the intracranial contents affect the Intracranial Pressure (ICP). Normal ICP is <15 mm Hg and is determined by the volume of the three intracranial compartments: the brain parenchyma (1300 ml), cerebrospinal fluid (CSF) (100 to 150 ml), and intravascular blood (100 to 150 ml). When one compartment expands, there is a compensatory reduction in the volume of another and/or the baseline ICP will increase (Monroe Kellie Hypothesis).[2] Rapid rises in ICP may lead to a phenomenon known as the Cushing Reflex (hypertension, bradycardia, and respiratory irregularity). This triad is classic for an acute rise in ICP. [3] If ICP rises to the level of the systemic arterial pressure, cerebral brain perfusion ceases and brain death occurs. Uncontrollable ICP is defined as an ICP of 20 mm Hg or higher refractory to treatment. If ICP is not controlled, herniation syndromes can occur, resulting in brainstem compression and subsequent cardiorespiratory arrest. [4] Of the various traditional means of detecting EICP in an acutely ill patient, none except physical examination can be performed rapidly and non-invasively at bedside. However, the physical examination has significant limitations if the patient is unconscious or intubated and paralyzed. Papilledema from EICP is delayed in its appearance from Intracranial Pressure Elevation, by up to several hours. Performing a lumbar puncture to measure pressure on a patient with potentially EICP may be dangerous. Thus, for most patients in the Emergency Department setting, Head Contrast Tomography scanning is often the best option available for the detection of EICP.
In situations like a disaster scene where multiple casualties are being triaged, and the ability to detect EICP in one out of several critical patients may help select the patient requiring the most rapid care also in times of scarce resources, when a decision has to be made regarding which trauma victim is most likely to survive.[5]
Ultrasound is a readily available imaging modality in most critical care areas, and examination of the optic nerve sheath by bedside ultrasound allows detection of changes in diameter which may indicate intracranial hypertension.[6]
Elevated ICP is a common emergency following brain injury, with prompt diagnosis having a significant impact on morbidity
 mm. The sensitivity and specificity for ONSD, when compared
with CT results, were 100% and 95%, respectively.
In Geeraerts et al [15] study the largest ONSD value was
significantly higher in EICP patients. There was a significant
relationship between the largest ONSD and ICP at admission.
The largest ONSD was a suitable predictor of high ICP.ONSD
was well prognosticated with treatment modalities. The
sensitivity was 100%.
mm. The sensitivity and specificity for ONSD, when compared
with CT results, were 100% and 95%, respectively.
In Geeraerts et al [15] study the largest ONSD value was
significantly higher in EICP patients. There was a significant
relationship between the largest ONSD and ICP at admission.
The largest ONSD was a suitable predictor of high ICP.ONSD
was well prognosticated with treatment modalities. The
sensitivity was 100%.
In Claire Shevlin et al [4] study of ONSD values greater than 5 mm, and certainly greater than 5.8 mm, have been shown to be highly specific and sensitive for the presence of EICP. EICP should be considered in the presence of an ONSD greater than 5mm, and if greater than 5.5 mm urgent consideration should be given to medical management.
Tayal et al[7], 59 patients were selected for the study, cutoff was kept to be 5 mm. Patients with EICP had ONSD > 5.5 mm. 8 patients with an ONSD of 5 mm or more had CT findings suggestive of EICP. Sensitivity 100%, specificity 63%.
Altered sensorium and focal neurological signs also showed significance with clinical correlation.92.31% patients having bradycardia had increased ONSD and abnormal CT findings.
51.02% patients having Irregular respiratory pattern had increased ONSD and abnormal CT findings.100% patients having a poor GCS between 3-8, had increased ONSD and abnormal CT findings.76.92% patients having a Moderate GCS between 9-12, had increased ONSD and abnormal CT findings.
CONCLUSION:
92.86% patients had ONSD >/=6 mm and abnormal CT Brain findings.
100%patients had ONSD between 5.5 to 5.9 mm and abnormal CT findings.
There were no patients having ONSD in ranges between 3.5 to 4.4 mm and 4.5 to 5.4 mm with abnormal CT findings (0.00%).
Elevated ICP should be considered in the presence of an ONSD greater than 5.5 mm, and if greater than 6 mm, urgent consideration should be given to medical management pending further diagnostic workup.
A poor GCS at the time of presentation to the ED is associated with Elevated ICP and has Increased ONSD with abnormal CT findings.
Bradycardia, Hypertension and Irregular breathing pattern are associated with Elevated ICP with Increased ONSD and abnormal CT findings. This defines the Cushings Reflex. 93.10% patients who had Increased ONSD and were started on Medical Management had EICP confirmed on CT Brain and Definitive treatment given.
ONSD value can thus be prognosticated with Treatment.
Thus Increased ONSD and Abnormal findings on CT scan Brain are statistically significant with Elevated ICP.
Bedside ultrasound has the advantages of Expense, time-effective, non-invasive and does not require moving a critical patient from the ED. In acute care settings, Ultrasound can be used for early detection and to prioritize patients in the setting of trauma. It is a rapid and reproducible modality and the method could be applied as an additional diagnostic tool in Emergency and Intensive care settings.
List of Figures;
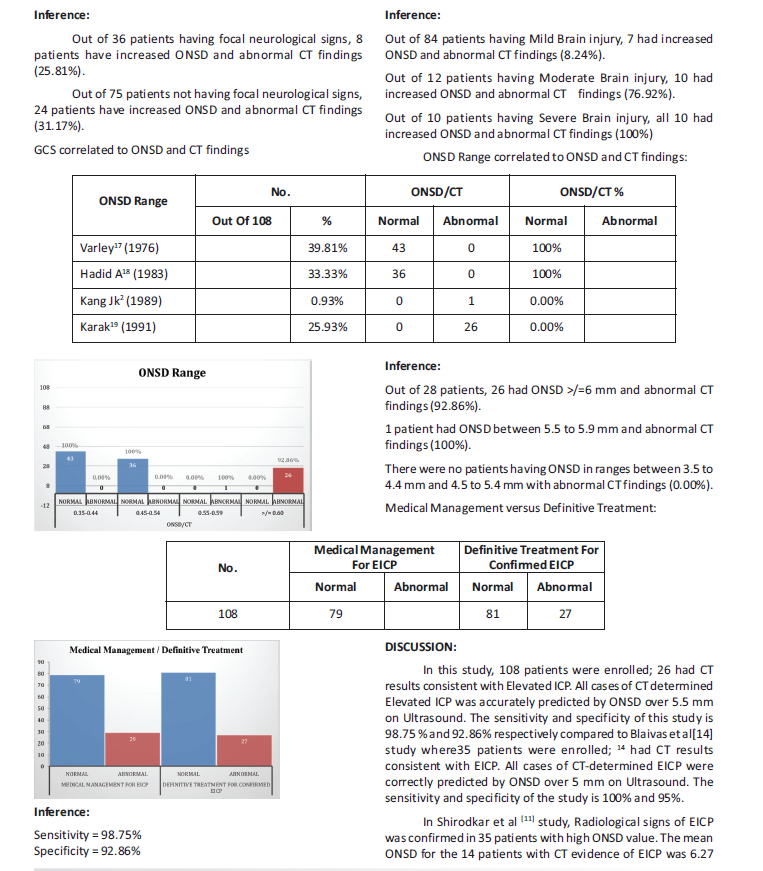
1. Proper transducer placement to obtain transverse & saggital 2. Measured increased ONSD
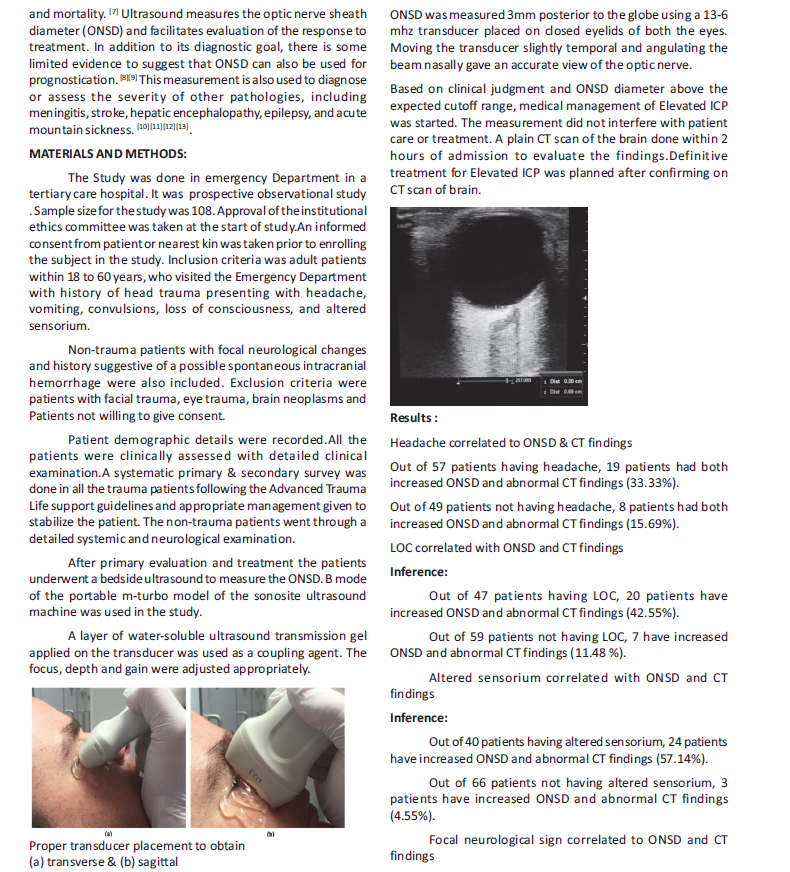
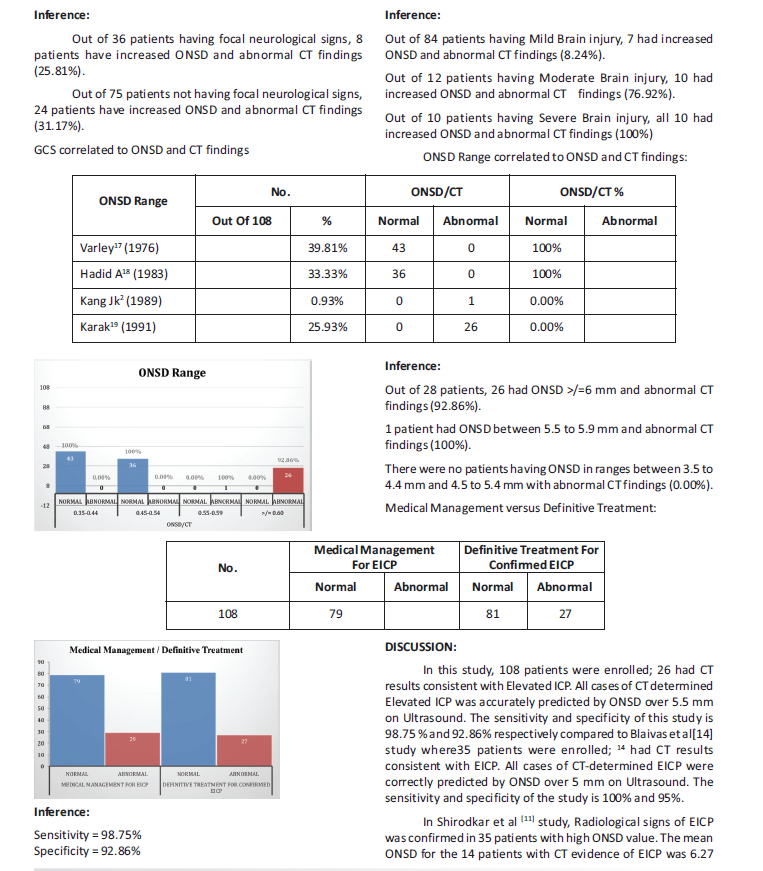
List of Tables:
1. ONSD range correlated to ONSD and Ct findings 2. Medical Management vs Definitive Treatment
REFERENCES:
1. Centers for Disease Control and Prevention: Vital Statistics. Available at: http:// www.cdc.gov/nchs/vitalstats.htm. Accessed December 22, 2008.
2. Robertson CS: Management of cerebral perfusion pressure after traumatic brain injury. Anesthesiology 95(6): 1513, 2001.
3. Hovda DA: Oxidative need and oxidative capacity following traumatic brain injury. Crit Care Med 35(2): 663, 2007.
4. Chesnut RM: Care of central nervous system injuries. Surg Clin North ?Am 2007; 87:119-156, vii.
5. Shevlin C. Optic Nerve Sheath Ultrasound for the Bedside Diagnosis of Intracranial Hypertension: Pitfalls and Potential. Critical Care Horizons 2015; 1: 22-30.?
6. Hayreh SS. Pathogenesis o edema of the optic disc. Doc Ophthalmol. 1968; 24:289-411.
7. Tayal VS, Neulander M, Norton HJ, Foster T, Saunders T, Blaivas M. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med. 2007;49(4):508–514.
8. Hwan Kim Y, Ho Lee J, Kun Hong C,Won Cho K, Hoon Yeo J, Ju Kang M, et al. Feasibility of optic nerve sheath diameter measured on initial brain computed tomography as an early neurologic outcome predictor after cardiac arrest. Acad Emerg Med. 2014;21(10):1121–1128.
9. Legrand A, Jeanjean P, Delanghe F, Peltier J, Lecat B, Dupont H. Estimation of optic nerve sheath diameter on an initial brain computed tomography scan can contribute prognostic information in traumatic brain injury patients. Crit Care. 2013;17(2):R61.
10. Nabeta HW, Bahr NC, Rhein J, Fossland N, Kiragga AN, Meya DB, et al. Accuracy of noninvasive intraocular pressure or optic nerve sheath diameter measurements for predicting elevated intracranial pressure in cryptococcal meningitis. Open Forum Infect Dis. 2014;1(3):ofu093.
11. Shirodkar CG, Rao SM, Mutkule DP, Harde YR, Venkategowda PM, Mahesh MU. Optic nerve sheath diameter as a marker for evaluation and prognostication of intracranial pressure in Indian patients: An observational study. Indian J Crit Care Med. 2014;18(11):728–734.
12. Kim YK, Seo H, Yu J, Hwang GS. Noninvasive estimation of raised intracranial pressure using ocular ultrasonography in liver transplant recipients with acute liver failure -A report of two cases-. Korean J Anesthesiol. 2013;64(5):451–455.
13. Manno E, Motevallian M, Mfochive A, Navarra M. Ultrasonography Of The Optic Nerve Sheath Suggested Elevated Intracranial Pressure In Epilepsy: Case Report. Internet J Anesthesiol. 2013;26(1).
14. Blaivas M, Theodoro D, Sierzenski PR. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med. 2003;10(4):376–381.
15. Geeraerts T, Launey Y, Martin L, Pottecher J, Vigué B, Duranteau J, et al. Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med. 2007;33(10):1704–1711.
16. Qayyum H, Ramlakhan S. Eur J Emerg Med. 2013 Apr;20(2):91-7. Doi: 10.1097/MEJ
How to cite this article : Mhatre M, Baviskar A, Dongre H, Rajpal D. Efficacy of optic nerve sheath diameter by ultrasound as a non-invasive method to determine elevated intracranial pressure in Indian population. Perspectives in Medical Research 2019; 7(2):38-42
Sources of Support: Nil,Conflict of interest:None declared
Year : 2019 | Volume : 7 | Issue : 2 Page : 38-42
Mhatre M1, Baviskar A2Dongre H3, Rajpal D4
*Address for correspondence:: Dr Ajit Baviskar, Department of Emergency Medicine, Dr. D.Y. Patil Medical College, Navi Mumbai.
E mail ID: - [email protected]
Introduction:
It is important to assess use of Optic Nerve sheath Diameter (ONSD) measurement by point of care ultrasonography (POCUS) as a non-invasive method for detecting elevated Intracranial Pressure (ICP) and to compare with Brain Computed Tomography (CT) findings of Elevated ICP in Indian population Methods:
This study was a Prospective Observational Study done in emergency Department of a tertiary care hospital in western India .Adult patients within 18-60 years age group, with Head trauma presenting with headache, vomiting, convulsions, loss of consciousness, and altered sensorium were included in the study.Non-trauma patients with focal neurological changes and history suggestive of possible spontaneous intracranial hemorrhage were also included. Data was recorded after stabilizing patients as per standard trauma and non-trauma protocol.
Patients underwent a POCUS study to measure the ONSD. Based on clinical judgment and ONSD measurement above the expected cut-off range, medical management for Elevated ICP was started. A Plain Brain CT Scan was obtained. Definitive treatment was planned after confirming on CT scan. ONSD measurement more than 6mm was suggestive of Elevated ICP Results:
108 patients were studied. A normal range of ONSD found was 3.5mm – 5.4mm.
26 patients had CT results consistent with Elevated ICP. All cases of CT-determined Elevated ICP were correctly predicted by ONSD. The sensitivity and specificity of this study is 98.75 % and 92.86% respectively.
Conclusion:
POCUS has the advantages of cost, time effective, non-invasive and reproducibility. It can be used as an additional diagnostic tool.
Keywords:
Optic nerve sheath diameter, Point of care Ultrasound, Intracranial pressure INTRODUCTION
Traumatic Brain Injury (TBI) is defined as impairment in brain function as a result of mechanical force. The dysfunction can be temporary or permanent, and may or may not result in underlying structural changes in the brain. [1] Any changes to the volume of the intracranial contents affect the Intracranial Pressure (ICP). Normal ICP is <15 mm Hg and is determined by the volume of the three intracranial compartments: the brain parenchyma (1300 ml), cerebrospinal fluid (CSF) (100 to 150 ml), and intravascular blood (100 to 150 ml). When one compartment expands, there is a compensatory reduction in the volume of another and/or the baseline ICP will increase (Monroe Kellie Hypothesis).[2] Rapid rises in ICP may lead to a phenomenon known as the Cushing Reflex (hypertension, bradycardia, and respiratory irregularity). This triad is classic for an acute rise in ICP. [3] If ICP rises to the level of the systemic arterial pressure, cerebral brain perfusion ceases and brain death occurs. Uncontrollable ICP is defined as an ICP of 20 mm Hg or higher refractory to treatment. If ICP is not controlled, herniation syndromes can occur, resulting in brainstem compression and subsequent cardiorespiratory arrest. [4] Of the various traditional means of detecting EICP in an acutely ill patient, none except physical examination can be performed rapidly and non-invasively at bedside. However, the physical examination has significant limitations if the patient is unconscious or intubated and paralyzed. Papilledema from EICP is delayed in its appearance from Intracranial Pressure Elevation, by up to several hours. Performing a lumbar puncture to measure pressure on a patient with potentially EICP may be dangerous. Thus, for most patients in the Emergency Department setting, Head Contrast Tomography scanning is often the best option available for the detection of EICP.
In situations like a disaster scene where multiple casualties are being triaged, and the ability to detect EICP in one out of several critical patients may help select the patient requiring the most rapid care also in times of scarce resources, when a decision has to be made regarding which trauma victim is most likely to survive.[5]
Ultrasound is a readily available imaging modality in most critical care areas, and examination of the optic nerve sheath by bedside ultrasound allows detection of changes in diameter which may indicate intracranial hypertension.[6]
Elevated ICP is a common emergency following brain injury, with prompt diagnosis having a significant impact on morbidity
 mm. The sensitivity and specificity for ONSD, when compared
with CT results, were 100% and 95%, respectively.
In Geeraerts et al [15] study the largest ONSD value was
significantly higher in EICP patients. There was a significant
relationship between the largest ONSD and ICP at admission.
The largest ONSD was a suitable predictor of high ICP.ONSD
was well prognosticated with treatment modalities. The
sensitivity was 100%.
mm. The sensitivity and specificity for ONSD, when compared
with CT results, were 100% and 95%, respectively.
In Geeraerts et al [15] study the largest ONSD value was
significantly higher in EICP patients. There was a significant
relationship between the largest ONSD and ICP at admission.
The largest ONSD was a suitable predictor of high ICP.ONSD
was well prognosticated with treatment modalities. The
sensitivity was 100%.In Claire Shevlin et al [4] study of ONSD values greater than 5 mm, and certainly greater than 5.8 mm, have been shown to be highly specific and sensitive for the presence of EICP. EICP should be considered in the presence of an ONSD greater than 5mm, and if greater than 5.5 mm urgent consideration should be given to medical management.
Tayal et al[7], 59 patients were selected for the study, cutoff was kept to be 5 mm. Patients with EICP had ONSD > 5.5 mm. 8 patients with an ONSD of 5 mm or more had CT findings suggestive of EICP. Sensitivity 100%, specificity 63%.
Altered sensorium and focal neurological signs also showed significance with clinical correlation.92.31% patients having bradycardia had increased ONSD and abnormal CT findings.
51.02% patients having Irregular respiratory pattern had increased ONSD and abnormal CT findings.100% patients having a poor GCS between 3-8, had increased ONSD and abnormal CT findings.76.92% patients having a Moderate GCS between 9-12, had increased ONSD and abnormal CT findings.
CONCLUSION:
92.86% patients had ONSD >/=6 mm and abnormal CT Brain findings.
100%patients had ONSD between 5.5 to 5.9 mm and abnormal CT findings.
There were no patients having ONSD in ranges between 3.5 to 4.4 mm and 4.5 to 5.4 mm with abnormal CT findings (0.00%).
Elevated ICP should be considered in the presence of an ONSD greater than 5.5 mm, and if greater than 6 mm, urgent consideration should be given to medical management pending further diagnostic workup.
A poor GCS at the time of presentation to the ED is associated with Elevated ICP and has Increased ONSD with abnormal CT findings.
Bradycardia, Hypertension and Irregular breathing pattern are associated with Elevated ICP with Increased ONSD and abnormal CT findings. This defines the Cushings Reflex. 93.10% patients who had Increased ONSD and were started on Medical Management had EICP confirmed on CT Brain and Definitive treatment given.
ONSD value can thus be prognosticated with Treatment.
Thus Increased ONSD and Abnormal findings on CT scan Brain are statistically significant with Elevated ICP.
Bedside ultrasound has the advantages of Expense, time-effective, non-invasive and does not require moving a critical patient from the ED. In acute care settings, Ultrasound can be used for early detection and to prioritize patients in the setting of trauma. It is a rapid and reproducible modality and the method could be applied as an additional diagnostic tool in Emergency and Intensive care settings.
List of Figures;
1. Proper transducer placement to obtain transverse & saggital 2. Measured increased ONSD
List of Tables:
1. ONSD range correlated to ONSD and Ct findings 2. Medical Management vs Definitive Treatment
REFERENCES:
1. Centers for Disease Control and Prevention: Vital Statistics. Available at: http:// www.cdc.gov/nchs/vitalstats.htm. Accessed December 22, 2008.
2. Robertson CS: Management of cerebral perfusion pressure after traumatic brain injury. Anesthesiology 95(6): 1513, 2001.
3. Hovda DA: Oxidative need and oxidative capacity following traumatic brain injury. Crit Care Med 35(2): 663, 2007.
4. Chesnut RM: Care of central nervous system injuries. Surg Clin North ?Am 2007; 87:119-156, vii.
5. Shevlin C. Optic Nerve Sheath Ultrasound for the Bedside Diagnosis of Intracranial Hypertension: Pitfalls and Potential. Critical Care Horizons 2015; 1: 22-30.?
6. Hayreh SS. Pathogenesis o edema of the optic disc. Doc Ophthalmol. 1968; 24:289-411.
7. Tayal VS, Neulander M, Norton HJ, Foster T, Saunders T, Blaivas M. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med. 2007;49(4):508–514.
8. Hwan Kim Y, Ho Lee J, Kun Hong C,Won Cho K, Hoon Yeo J, Ju Kang M, et al. Feasibility of optic nerve sheath diameter measured on initial brain computed tomography as an early neurologic outcome predictor after cardiac arrest. Acad Emerg Med. 2014;21(10):1121–1128.
9. Legrand A, Jeanjean P, Delanghe F, Peltier J, Lecat B, Dupont H. Estimation of optic nerve sheath diameter on an initial brain computed tomography scan can contribute prognostic information in traumatic brain injury patients. Crit Care. 2013;17(2):R61.
10. Nabeta HW, Bahr NC, Rhein J, Fossland N, Kiragga AN, Meya DB, et al. Accuracy of noninvasive intraocular pressure or optic nerve sheath diameter measurements for predicting elevated intracranial pressure in cryptococcal meningitis. Open Forum Infect Dis. 2014;1(3):ofu093.
11. Shirodkar CG, Rao SM, Mutkule DP, Harde YR, Venkategowda PM, Mahesh MU. Optic nerve sheath diameter as a marker for evaluation and prognostication of intracranial pressure in Indian patients: An observational study. Indian J Crit Care Med. 2014;18(11):728–734.
12. Kim YK, Seo H, Yu J, Hwang GS. Noninvasive estimation of raised intracranial pressure using ocular ultrasonography in liver transplant recipients with acute liver failure -A report of two cases-. Korean J Anesthesiol. 2013;64(5):451–455.
13. Manno E, Motevallian M, Mfochive A, Navarra M. Ultrasonography Of The Optic Nerve Sheath Suggested Elevated Intracranial Pressure In Epilepsy: Case Report. Internet J Anesthesiol. 2013;26(1).
14. Blaivas M, Theodoro D, Sierzenski PR. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med. 2003;10(4):376–381.
15. Geeraerts T, Launey Y, Martin L, Pottecher J, Vigué B, Duranteau J, et al. Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med. 2007;33(10):1704–1711.
16. Qayyum H, Ramlakhan S. Eur J Emerg Med. 2013 Apr;20(2):91-7. Doi: 10.1097/MEJ
How to cite this article : Mhatre M, Baviskar A, Dongre H, Rajpal D. Efficacy of optic nerve sheath diameter by ultrasound as a non-invasive method to determine elevated intracranial pressure in Indian population. Perspectives in Medical Research 2019; 7(2):38-42
Sources of Support: Nil,Conflict of interest:None declared
Open Access
Perspectives in Medical Research is committed to keeping research articles Open Access.Journal permits any users to read, download, copy, print, search, or link to the full texts of these articles...
Read more
© PIMR.org.in - 2013. All Rights Reserved.
