Volume: 13 Issue: 3
Exploring Tuberculosis Awareness Among Future Healthcare Providers in Tertiary Healthcare Centre.
Year: 2025, Page: 203-207, Doi: https://doi.org/10.47799/pimr.1303.25.58
Received: Sept. 5, 2025 Accepted: Dec. 16, 2025 Published: Dec. 31, 2025
Abstract
Introduction: Tuberculosis (TB) remains a global health threat, with India contributing significantly to the burden. The National Tuberculosis Elimination Programme (NTEP) aims to eliminate TB by 2025. A key factor in achieving this goal is the level of awareness and knowledge about TB among medical students, who play a crucial role in diagnosing, managing the disease and treating patients. Objective: This study aims to assess the TB-related knowledge of medical students in India. Methods: A prospective cross-sectional study was conducted among 500 MBBS students at a Government Medical College for three months duration. Data was collected via a structured questionnaire that assessed knowledge on TB epidemiology, diagnosis, treatment, and the NTEP facilities available at the hospital. The responses were analyzed. Correct answers were mailed to students. Results: Out of 500 students, 103 responded to the survey. 74.76% of respondents had adequate knowledge about TB, with 26.21% demonstrating thorough knowledge. Knowledge was positively correlated with the students' academic year, with older students showing a better understanding of the disease. A gap in knowledge was identified regarding diagnostic methods, especially confirmatory tests and drug-resistant TB management. Conclusion: The study found that while medical students in India show a reasonable level of awareness about TB, significant gaps remain in diagnostic knowledge. Strengthening educational interventions focused on diagnostic skills and TB management is essential. Addressing these gaps is crucial for enhancing TB care and achieving the goals of NTEP by 2025.
Keywords: Medical students, NTEP, Questionnaire, Tuberculosis
INTRODUCTION
According to World Health Organization (WHO), Tuberculosis (TB) continues to be a significant global health concern, despite being a preventable and treatable disease.[1] In 2022, TB remained the second leading cause of death from a single infectious agent, after COVID-19, and was responsible for nearly twice as many deaths as HIV/AIDS. India alone bears a one-quarter of the global TB burden.[1] Over 10 million people are affected by TB each year, with staggering number of fatalities occurring primarily in low- and middle-income countries.[2]
In response, India’s National Tuberculosis Elimination Programme (NTEP) has made substantial progress in improving TB care and treatment, including efforts to tackle drug-resistant TB (DR-TB). Since 2017, NTEP has introduced several key strategies, including the rollout of new diagnostic technologies, treatment regimens, and patient-centered care models, all aimed at accelerating TB control. [3] Despite these efforts, gaps in knowledge about TB persist, especially among healthcare professionals, which can affect the quality of care provided and the overall effectiveness of TB control programs. [4]
Medical students, as future healthcare providers, are crucial to the success of TB elimination efforts. They are often at the forefront of diagnosing, treating, and educating patients about TB. However, studies have shown that medical students may have limited knowledge about the disease, its transmission, and effective prevention strategies, which could hinder the management of TB at the clinical level. [5] Additionally, misconceptions about TB treatment, particularly in relation to drug-resistant strains, have been reported among healthcare students, potentially contributing to delays in diagnosis and inappropriate treatment practices. [6]
This study aims to assess the level of awareness and knowledge of TB among medical students in India, focusing on critical aspects such as its transmission, prevention, and treatment. By evaluating their current understanding and identifying knowledge gaps, this research seeks to inform targeted educational interventions that can enhance TB awareness and, ultimately, contribute to India's broader goal of TB elimination. [7]
MATERIALS AND METHODS
A prospective cross-sectional study was conducted to evaluate the level of awareness and knowledge about tuberculosis (TB) among 500 MBBS students (250 students of second year MBBS, 250 of third year MBBS) at a government medical college, affiliated with a tertiary care hospital. The study took place over a two-month period, from 26th October 2023 to 26th December 2023. The primary aim was to assess medical students' understanding of key aspects of TB, including its epidemiology, diagnosis, treatment, and the resources available under the National Tuberculosis Elimination Programme (NTEP) at the associated tertiary hospital.
Inclusion criteria- Only second and third MBBS students were included in study.
Exclusion criteria- MBBS students have detailed syllabus on TB in second year, so first year students were excluded. Also, final MBBS students were busy in their exam they were also excluded. Interns, Post graduate Residents and faculty members were also excluded.
Study Design and Participants
The study targeted MBBS students enrolled in various phases of their medical education. A total of 500 students participated in the study, providing a broad sample of current medical students. Ethical approval for the study was obtained from the institutional review board of the medical college, ensuring that all participants voluntarily participated and gave informed consent. To maintain confidentiality, the survey was anonymous. The validation of study was taken from Head of department of Microbiology and Pulmonary Medicine. For conducting pilot study, 10 medical students were asked to solve questionnaire. The questionnaire was standardized as all participants were asked identical questions and responses were recorded in uniform manner.
Questionnaire Design
The data collection was carried out using a structured questionnaire, which was divided into four key sections to assess the students' knowledge about TB:
-
Disease Knowledge (5 questions):
This section aimed to evaluate the students' basic understanding of tuberculosis, including its causative organism (Mycobacterium tuberculosis), modes of transmission, risk factors, and global burden. Questions also assessed students' familiarity with the clinical presentation of TB, including common symptoms and signs that could lead to early diagnosis. -
Laboratory Diagnosis of TB (8 questions):
The focus of this section was to assess the students' awareness of the various diagnostic modalities available for TB, such as sputum smear microscopy, chest X-ray, and advanced molecular techniques like GeneXpert and PCR-based tests. It also explored their understanding of the importance of drug susceptibility testing, especially in the context of drug-resistant TB (DR-TB), and the protocols for accurate diagnosis. -
NTEP Facilities at the Associated Tertiary Hospital (3 questions):
This segment aimed to gauge the students’ knowledge of the National Tuberculosis Elimination Programme (NTEP) and its infrastructure at the affiliated hospital. It included questions on the availability of TB-related diagnostic tools, treatment regimens, and patient support services. Additionally, students were asked about their awareness of the role of NTEP in managing drug-resistant TB and ensuring comprehensive patient care. -
Management and Treatment (4 questions):
The final section of the questionnaire focused on students’ understanding of the management and treatment strategies for TB. This included questions on the standard first-line and second-line drug regimens, the importance of adherence to treatment, and the challenges posed by multi-drug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB). The students’ knowledge of the duration of treatment and monitoring of TB patients was also assessed.
Data Collection Process
The questionnaire was distributed online via Google Sheets to all the participants. The online format allowed for easy distribution and ensured that students could complete the survey at their convenience within the given time frame. Each participant was asked to respond to the questions independently (self-administered), ensuring that their answers reflected their personal understanding of the subject. Time given to solve them was 20 minutes.
Once all responses were submitted, the collected data were organized and analyzed. Each participant’s responses were reviewed for completeness and accuracy. Descriptive statistical methods were used to analyze the data, identifying trends in knowledge and areas where gaps were most prominent. The data were also categorized by academic year to assess whether there were differences in knowledge based on the students' progression in their medical studies.
Post-Survey Feedback
After the analysis of the responses, an answer key was compiled and emailed to each participant to provide feedback on their performance. This feedback aimed to reinforce correct knowledge and address common misconceptions. By offering this follow-up, the study also sought to enhance learning and awareness of TB, ensuring that students had access to accurate information and could identify areas for improvement.
RESULTS
A total of 500 students were requested to take part in the survey out of which 103 students responded. Out of these responses, 85 responses (82.52%) were from 2nd year MBBS students and 18 were from third year (17.47%). 83 of these responses (80.58%) were by students above the age of 20 (20-23 years of age) and 20 responses (19.42%) were below 20 years of age.
Out of a total of 103 responses, 85 responses were from second year students and 18 were by third year students. 77 respondents (74.76%) had adequate knowledge about tuberculosis [Fig. 1] (score above 50%) while only 27 respondents(26.21%) had thorough knowledge (score above 75%). [Fig. 1] Older medical students had a more thorough knowledge about TB compared to the younger ones.
[Fig. 2] [Fig. 3] and [Fig. 4] describes knowledge regarding Laboratory diagnosis, NTEP and treatment respectively.
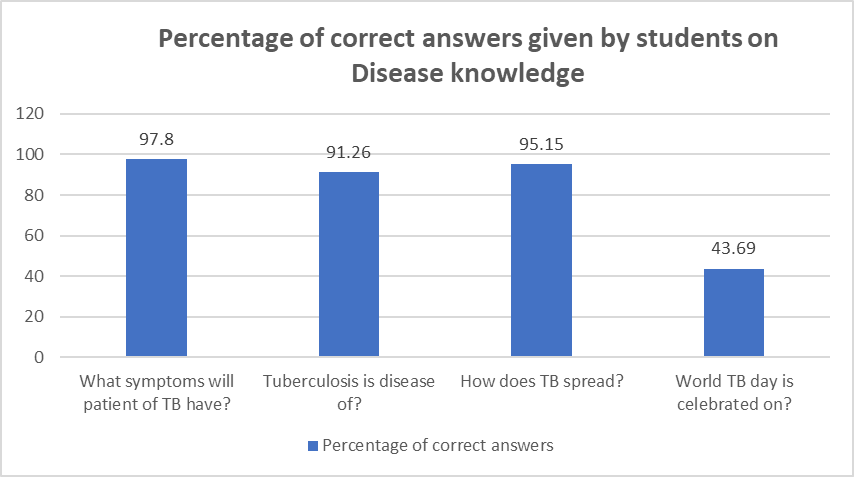
Figure 1: Percentage of correct answers given by students on Disease knowledge
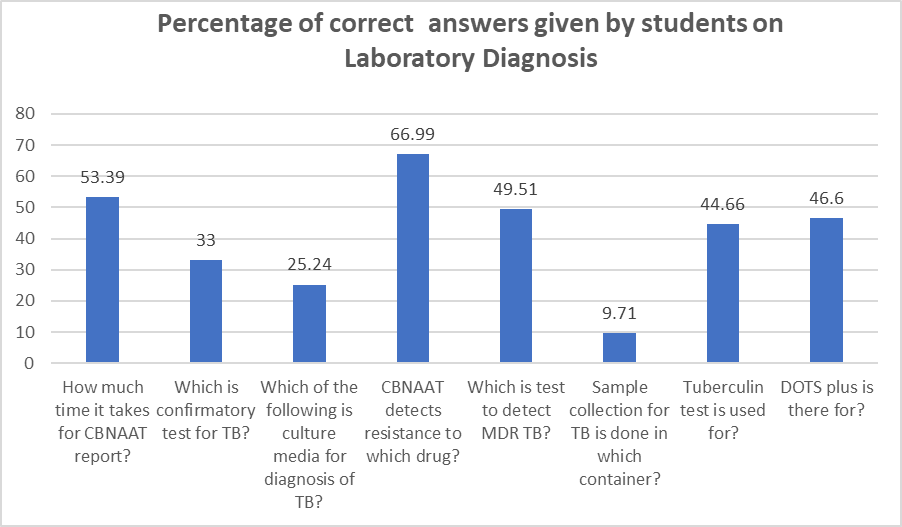
Figure 2: Percentage of correct answers given by students on Laboratory Diagnosis
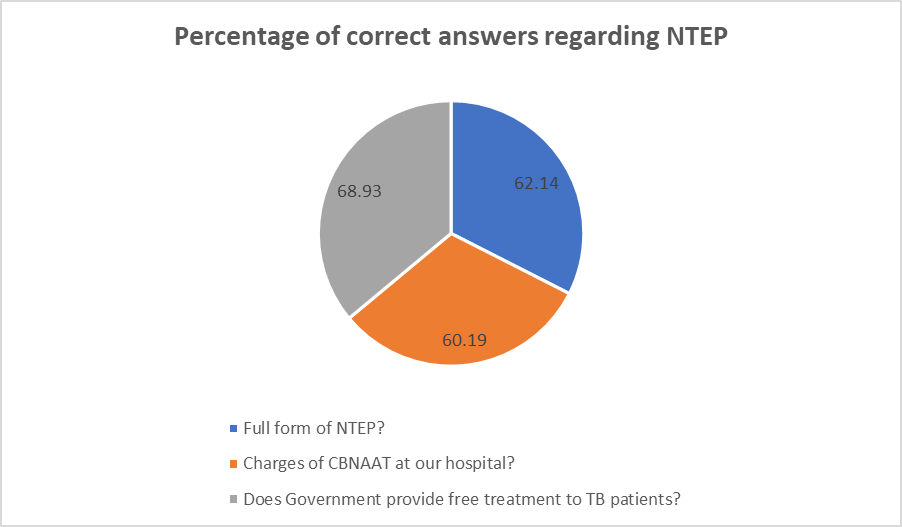
Figure 3: Percentage of correct answers given by students regarding NTEP
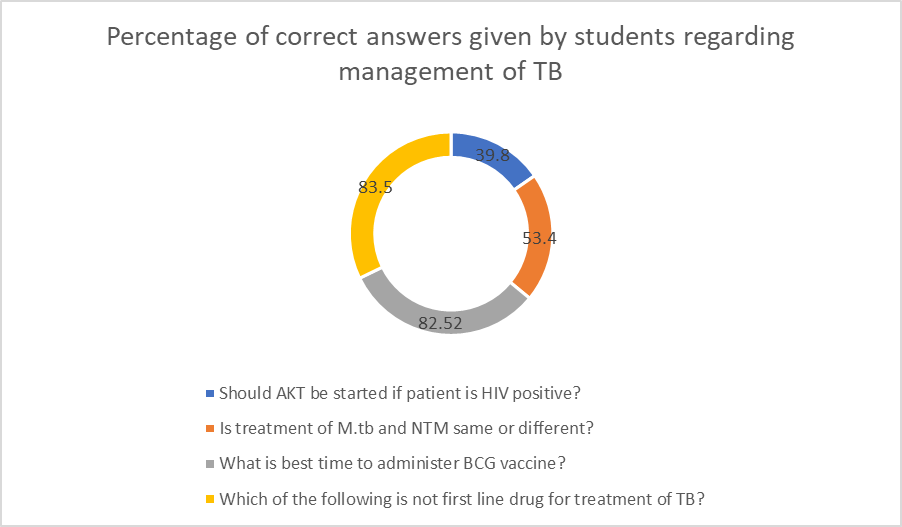
Figure 4: Percentage of correct answers given by students regarding management of TB
DISCUSSION
In present study. the participants' ages ranged from 19 to 23 years. However, the response rate was notably low at 20.6%, primarily due to hesitancy among students to participate and their demanding academic schedules. In a study conducted by Li-Qiong Bai et al., the response rate was exceptionally high at 97.6%. Despite this, only 25.5% of participants were aware of the BCG vaccination, and a mere 16.8% knew about the standard TB treatment regimen. [8] In contrast, our study revealed that 81.5% of participants were aware of the BCG vaccine, and 67.3% were knowledgeable about the treatment regimen.
A study conducted by Yangjiang Ou et al., in Hunan Province, China, reported a total mean percentage of TB knowledge among medical students at 44.4%, with specific scores of 35.7% for diagnosis and 47.5% for treatment. [9] In our study, the total mean percentage of TB knowledge was 60%, with 50.6% for diagnosis and 67.3% for treatment. [Fig. 1]
The study by Yangjiang Ou et al. also highlighted that older medical students (≥23 years) had greater knowledge about TB compared to younger students (<23 years). [9] This finding aligns with our study's observations, suggesting that increased exposure and experience contribute to enhanced TB knowledge among medical students.
A study conducted by Eleny Guimaraes Teixeira et al., in Rio de Janeiro revealed that 52.6% of medical students were aware of the modes of tuberculosis transmission, specifically recognizing that the disease spreads through coughing, sneezing, and speaking . [10] In our study, while students demonstrated a reasonable understanding of transmission routes, there was a noticeable gap in knowledge concerning diagnostic procedures. Many students struggled to identify confirmatory tests for tuberculosis, the application of the tuberculin skin test, and the use of liquid media for culturing Mycobacterium tuberculosis.
These findings align with other studies highlighting deficiencies in diagnostic knowledge among medical students. For instance, a survey among medical students in Chennai reported that while 85% were aware of treatment options and drugs available for tuberculosis, only 70% had knowledge about diagnostic techniques. [11] Similarly, research in Tamil Nadu indicated that while 98% of students understood transmission routes and affected sites, only 70% were knowledgeable about diagnostic methods. [12]
These gaps underscore the necessity for enhanced educational strategies focusing on the diagnostic aspects of tuberculosis. Incorporating practical training, such as hands-on experience with diagnostic procedures and exposure to real-life cases, could significantly improve students' competence in this critical area.
Our study indicates a relatively high level of TB awareness among medical students in India, surpassing findings from similar studies in China. This underscores the effectiveness of TB education initiatives in Indian medical colleges. However, the low response rate highlights the need for strategies to encourage greater participation in such surveys. Future research should explore the underlying reasons for non-participation and develop interventions to address them, ensuring comprehensive assessment of TB knowledge among medical students.
CONCLUSION
This study highlights a moderate level of awareness and knowledge about tuberculosis among MBBS students, with 74.76% demonstrating adequate understanding and only 26.21% showing thorough knowledge (scoring above 75%). A significantly higher proportion of responses were received from second-year students, and the majority of participants were above 20 years of age. Findings indicate that older students and those in more advanced academic years tend to have better knowledge about TB, suggesting that increased exposure to clinical subjects and public health programs such as the National Tuberculosis Elimination Programme (NTEP) enhances understanding. However, the relatively low percentage of students with thorough knowledge underscores the need to integrate more comprehensive and structured TB-related content into the MBBS curriculum at earlier stages. This could improve the preparedness of future medical professionals in combating TB, especially in high-burden countries like India.
LIMITATIONS OF THE STUDY
A significant limitation of this study is the low response rate of 20.6%, which may not accurately represent the knowledge levels of all medical students. As this is single centred study, it is difficult to generalise the conclusions. Additionally, the study's cross-sectional design limits the ability to establish causal relationships between knowledge levels and other variables. As questionnaire was circulated through google sheet, online survey bias and response bias cannot be eliminated.
References
1. World Health Organization (WHO). Global Tuberculosis Report 2022. Geneva: WHO; 2022.
2. Central TB Division, Ministry of Health and Family Welfare. National Strategic Plan for Tuberculosis Elimination 2017–2025. New Delhi: Ministry of Health and Family Welfare; 2017.
3. Khanna A, Saha R, Ahmad N. National TB elimination programme - What has changed. Indian Journal of Medical Microbiology. 2023; 42 Available from: https://doi.org/10.1016/j.ijmmb.2022.10.008
4. Shah HD, Khatib NM, Syed ZQ, Gaidhane AM, Yasobant S, Narkhede K. Gaps and Interventions across the Diagnostic Care Cascade of TB Patients at the Level of Patient, Community and Health System: A Qualitative Review of the Literature. Tropical Medicine and Infectious Disease. 2022; 7 (7). Available from: https://doi.org/10.3390/tropicalmed7070136
5. Laurenti P, Federico B, Raponi M, Furia G, Ricciardi W, Damiani G. Knowledge, experiences, and attitudes of medical students in Rome about tuberculosis. Medical Science Monitor. 2013; 19 Available from: https://doi.org/10.12659/msm.889515
6. Teibo TKA, Andrade RLP, Rosa RJ, de Abreu PD, Olayemi OA, Alves YM, <i>et al</i>. Barriers That Interfere with Access to Tuberculosis Diagnosis and Treatment across Countries Globally: A Systematic Review. ACS Infectious Diseases. 2024; 10 (8). Available from: https://doi.org/10.1021/acsinfecdis.4c00466
7. Sharma N, Arora E, Lahariya C, Chopra KK. Competency based medical education as an accelerator to end tuberculosis (End TB) in India. Indian Journal of Tuberculosis. 2024; 71 (1). Available from: https://doi.org/10.1016/j.ijtb.2023.12.001
8. Bai L, Xiao S, Xie H, Yang G, Wang Y. Knowledge and practice regarding tuberculosis among final-year medical students in Hunan, China. China. Zhonghua Jie He He Hu Xi Za Zhi. 2003; 26 (8). Available from: https://pubmed.ncbi.nlm.nih.gov/14505520/
9. Ou Y, Luo Z, Mou J, Ming H, Wang X, Yan S, <i>et al</i>. Knowledge and determinants regarding tuberculosis among medical students in Hunan, China: a cross-sectional study. BMC Public Health. 2018; 18 (1). Available from: https://doi.org/10.1186/s12889-018-5636-x
10. Teixeira EG, Menzies D, Cunha AJL, Luiz RR, Ruffino-Netto A, Scartozzoni MS, <i>et al</i>. Knowledge and practices of medical students to prevent tuberculosis transmission in Rio de Janeiro, Brazil. Revista Panamericana de Salud Pública. 2008; 24 (4). Available from: https://doi.org/10.1590/s1020-49892008001000006
11. Manoharan A, Chellaiyan VG, Jasmine M, Liaquathali F. Impact of educational intervention on the tuberculosis knowledge among the medical students, Chennai. International Journal Of Community Medicine And Public Health. 2019; 6 (12). Available from: https://doi.org/10.18203/2394-6040.ijcmph20195491
12. Jha S, Shrivastava SR. A cross-sectional descriptive study to assess the awareness about tuberculosis, GeneXpert, Nikshay, and 99-DOTS among the representative population of medical students. Indian Journal of Health Sciences and Biomedical Research KLEU. 2024; 17 (1). Available from: https://doi.org/10.4103/kleuhsj.kleuhsj_470_23
Copyright
©2025 (Tappe) et al. This is an open-access journal, and articles are distributed under the terms of the Creative Commons Attribution License CC-BY 4.0. (https://creativecommons.org/licenses/by/4.0/) which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited.
Cite this article
Tappe A, Shah P, Pol S, Karyakarte R. Exploring Tuberculosis Awareness Among Future Healthcare Providers in Tertiary Healthcare Centre. Perspectives in Medical Research 2025;13(3):203-207 DOI: 10.47799/pimr.1303.25.58