Volume: 13 Issue: 3
Hansen’s Disease- A Comprehensive Study Through the Lens of Histopathology and Clinical Correlation: In a Teritiary Care Centre
Year: 2025, Page: 163-169, Doi: https://doi.org/10.47799/pimr.1303.25.54
Received: Aug. 27, 2025 Accepted: Nov. 3, 2025 Published: Dec. 31, 2025
Abstract
Introduction: Hansen’s disease is a chronic infectious disease caused by Mycobacterium leprae bacilli, primarily affecting the skin and peripheral nerves. Despite treatment with multidrug therapy (MDT), it remains a public health concern in many countries, particularly in South-East Asia. Early detection is essential to prevent the disease’s spread and disability. Due to the multiple morphologies, it may be difficult to accurately diagnose certain cases based solely on clinical signs; therefore, histopathology is crucial for definitive diagnosis. Objectives: To evaluate the clinical and histopathological correlation with their concordance rates thereby highlighting the role of histopathology in diagnosis and management, especially in borderline leprosy (Hansen’s disease) cases. Methods: A retrospective study was conducted at Malla Reddy Institute of Medical Sciences from October 2023 to March 2025. Fifty-two skin biopsies from clinically suspected leprosy cases were studied using Haematoxylin & Eosin and Fite-Faraco staining. Cases were classified histologically along with bacteriological index as per the Ridley-Jopling system. Concordance between clinical and histological diagnosis was statistically analysed. Results: Out of 52 cases, 61.5% were males, females contributing to 38.4%. The most affected age group was 21–30 years (46%). Histopathological types included Lepromatous Leprosy (LL) (42.3%), Borderline Lepromatous (BL) (21%), and Borderline Tuberculoid (BT) (15.3%). Overall concordance between clinical and histopathological classification was analysed statistically with highest agreement observed in TT (96.2%) and BT (94.2%) with a greater number of multibacillary cases showing acid-fast bacilli on Fite-Faraco staining. Conclusion: Accurate diagnosis using Ridley-Jopling classification integrates clinical, histological, and immunological findings which plays a pivotal role for effective management.
Keywords: Bacteriological index (BI), Fite-Faraco stain, Hansen’s disease, Ridley-Jopling classification
INTRODUCTION
Hansen’s disease is a chronic infectious disease caused by Mycobacterium leprae bacilli, primarily affecting the skin and peripheral nerves. Despite treatment with multidrug therapy (MDT), it remains a public health concern in many countries, particularly in South-East Asia. Accurate diagnosis using Ridley-Jopling classification integrates clinical, histological, and immunological findings. are essential for effective management.
As per data of 2023, Brazil, India and Indonesia continue to report more than 10 000 new cases, while 12 other countries (Bangladesh, Democratic Republic of Congo, Ethiopia, Madagascar, Mozambique, Myanmar, Nepal, Nigeria, Philippines, Somalia, Sri Lanka and the United Republic of Tanzania) each reported 1000–10,000 new cases 1.
The overall prevalence of leprosy in India declined from 5.27/10 000 in the year 2000 to 0.66/10 000 in the year 2016, but still, it continues to be a sizable public health problem 2.
With the availability of multiple drug therapy (MDT) as a cure for leprosy, the National Leprosy Eradication Program (NLEP) was launched in 1983–1984.
The NLEP’s mission is to supply quality leprosy services free of cost to many sections of the population with easy accessibility through the integrated healthcare system, including disability management post-cure of the disease 3.
According to World Health Organization (WHO), leprosy is still present in more than 120 countries and is a neglected tropical disease (NTD), with more than 2,00,000 new cases being reported annually 4.
National Strategic Plan (NSP) and Roadmap of Leprosy 2023-2027 5
NSP 2023-2027 is aligned with global strategy 2021-2030 6 and has a vision of Leprosy free India 7. It has a goal of accelerating the programme for interruption of transmission of leprosy by 2027 – three years ahead of sustainable development goal 3.3.
Therefore, early detection is essential to prevent the disease’s spread and disability. Accurate diagnosis using Ridley-Jopling classification integrates clinical, histological, and immunological findings which plays a pivotal role for effective management.
MATERIALS AND METHODS
Inclusion Criteria:
-
Patients of all age groups and all genders who have hypopigmented, hypoanaesthetic skin lesions.
-
Patients who are clinically diagnosed with Hansen’s disease.
-
Patients who give informed consent are willing to be part of study.
Exclusion Criteria:
-
Patients who are already diagnosed and on treatment for Hansen’s disease.
-
Patients who refuse to give consent for biopsy and HIV-positive cases, pregnant women, patients on immunosuppressive drugs.
-
All cases where the biopsy is inadequate will be excluded from the study.
Demographic data such as age, gender, and duration of symptoms were recorded. Detailed clinical examination was conducted and findings such as hypopigmented lesions, nerve involvement were recorded. Skin biopsy was performed from the most representative lesion under sterile conditions using local anaesthesia.
A 4–6 mm punch biopsy is preferred. The tissue is fixed in 10% formalin and transported to the histopathology laboratory.
Formalin-fixed tissue is processed, embedded in paraffin, and sectioned. The sections were stained using Haematoxylin and Eosin (H&E) for routine histopathological evaluation and Fite-Faraco staining for identifying the bacterial load and bacillary index (BI) are systematically documented based on the Ridley-Jopling classification 8.
Statistical Analysis
The data was analysed in SPSS for descriptive statistics. Frequencies, percentages are calculated for clinical variables. Clinical, histopathological, and bacteriological findings with statistical correlation are tabulated accordingly.
RESULTS
Total 52 leprosy cases were included. Male to female ratio was 1.3:1. Majority (53.8%; 28 cases) were between 21 – 40 yrs followed by 41 – 60 yrs (26.9%; 14 cases), 61-80 yrs (7.7%; 4 cases). Hypopigmented patches were seen in (32 cases -61.5%) cases followed by erythematous lesions (15 cases-28.8%) and nerve thickening (5 cases-9.6%).
Table 1: Distribution of cases according to Age and Sex
|
Age (Years) |
Male |
Female |
|
21-30 |
16 |
8 |
|
31-40 |
9 |
3 |
|
41-50 |
3 |
6 |
|
51-60 |
3 |
2 |
|
61-70 |
1 |
1 |
|
Total |
32 |
20 |
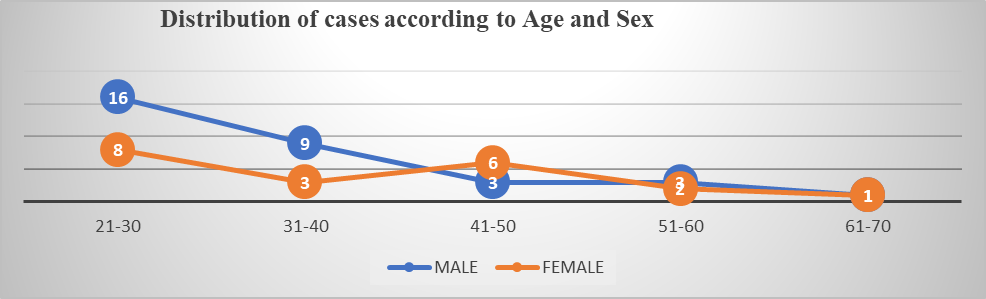
Figure 1: Distribution of cases according to Age and Sex

Figure 2: Hypopigmented patches

Figure 3: Erythematous plaques over back
When clinical and histopathological diagnoses was correlated, TT achieved 96% concordance rate with BT and BB showed 94% agreement, respectively. BL had 85%, while LL had an 81% match.
-
BT has the highest sensitivity (100%).
-
BB and IL show very high specificity (>97%).
Table 2: Bacteriological Index with each Histopathological type
|
Histological Type |
0 |
+1 |
+2 |
+3 |
+4 |
+5 |
+6 |
Total |
|
TT |
3 |
- |
- |
- |
- |
- |
- |
3 |
|
BT |
8 |
- |
- |
- |
- |
- |
- |
8 |
|
BB |
1 |
1 |
1 |
- |
- |
- |
- |
3 |
|
BL |
- |
- |
- |
2 |
5 |
4 |
- |
11 |
|
LL |
- |
- |
- |
2 |
8 |
7 |
5 |
22 |
|
IL |
4 |
1 |
- |
- |
- |
- |
- |
5 |
|
Total |
16 |
2 |
1 |
4 |
13 |
11 |
5 |
52 |
Table 3: Histopathological diagnosis of clinically diagnosed cases correlation
|
Clinical Diagnosis (N=52) |
Histopathological Diagnosis |
||||||
|
TT (N = 3) |
BT (N = 8) |
BB (N = 3) |
BL (N = 11) |
LL (N = 22) |
IL (N = 5) |
Total |
|
|
TT |
2 |
0 |
0 |
1 |
0 |
1 |
4 |
|
BT |
0 |
8 |
0 |
2 |
0 |
1 |
11 |
|
BB |
0 |
0 |
2 |
0 |
0 |
0 |
2 |
|
BL |
0 |
0 |
1 |
7 |
4 |
0 |
12 |
|
LL |
1 |
0 |
0 |
1 |
18 |
1 |
21 |
|
IL |
0 |
0 |
0 |
0 |
0 |
2 |
2 |
|
Total |
3 |
8 |
3 |
11 |
22 |
5 |
52 |
Table 4: Sensitivity, Specificity , Positive predictive value, Negative predictive value, Agreement value of clinically diagnosed cases in Our study
|
HPE Diagnosis |
Sensitivity (%) |
Specificity (%) |
PPV (%) |
NPV (%) |
Agreement % |
|
TT |
66.7% |
96.0% |
50.0% |
98.0% |
96.2% |
|
BT |
100.0% |
92.7% |
72.7% |
100.0% |
94.2% |
|
BB |
33.3% |
98.0% |
33.3% |
98.0% |
94.2% |
|
BL |
63.6% |
94.9% |
63.6% |
94.9% |
84.6% |
|
LL |
81.8% |
80.0% |
75.0% |
85.7% |
80.8% |
Table 5: Comparison of concordance rates of histopathological subtypes in our study with other studies
|
Leprosy subtypes |
Our study |
Atram, et.al 9 |
Kumar et al 10 |
Kini and Chaudhary 11 |
|
TT |
96.2% |
88.4 |
81.8 |
92.4 |
|
BT |
94.2% |
86.4 |
34.5 |
82 |
|
BB |
94.2% |
96.1 |
54.1 |
97.8 |
|
BL |
84.6% |
95.1 |
21.3 |
92.6 |
|
LL |
80.8% |
97.1 |
64.3 |
96.8 |
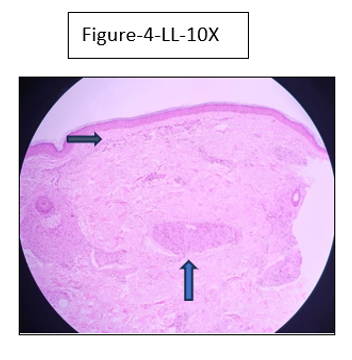
Figure 4: Lepromatous Leprosy (LL)-10x view- Atrophic epidermis with G renz zone, diffuse infiltration of foamy histiocytes
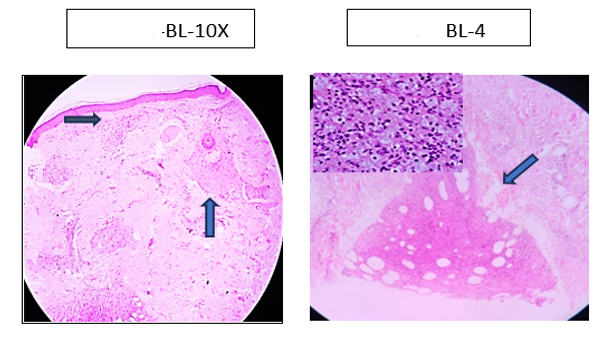
Figure 5: Borderline Leprosy (B L)-10x view- Macrophage granuloma with foamy macrophages (in the subset) and clear Grenz zone
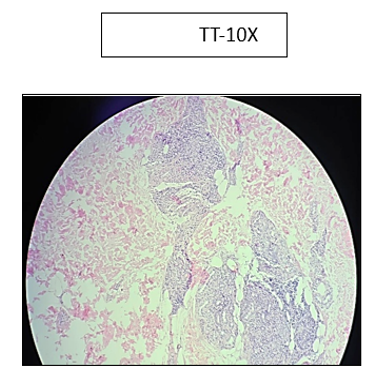
Figure 6: Tuberculosis Leprosy (TT)-10x view- Characteristic tuberculoid granuloma with epithelioid cells,

Figure 7: Tuberculosis Leprosy (TT)-40x view- F ew Langhan type giant cells surrounded by plenty of lymphocyres
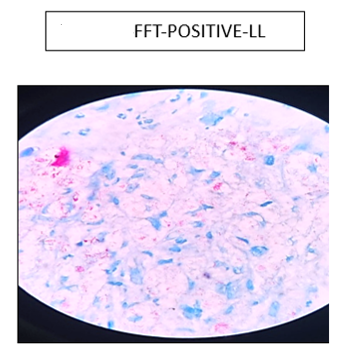
Figure 8: Fite Faraco stain showing lepra bacilli in globi (BI - + 4 to +5) in a case of Lepromatous Leprosy (LL)

Figure 9: Fite Faraco stain showing no lepra bacilli in globi (BI- 0 ) in a case of Tuberculoid Leprosy ( TT)
DISCUSSION
Our study of 52 clinically diagnosed leprosy cases were included with a male to female ratio of 1.3:1 showing concordance with study done by Archana, et.al 12- Leprosy occurs in all age groups and both genders but is known to have a propensity among adults with a male predominance (Table 1).
The age distribution revealed that most cases (53.8%) occurred in the 21 – 40 years age group, followed by 26.9% in the 41–60 years range in concordance with study by Atram et al 9. This age distribution and male preponderance can be due to variations in healthcare approach, occupational exposure, and immunological factors (Table 1, Figure 1).
In this study, hypopigmented patches were the most common clinical presentation, observed in 61.5% (32/52) of cases (Figure 2). Hypopigmented lesions are a hallmark of early leprosy, particularly in tuberculoid and borderline tuberculoid forms, due to localized immune responses leading to melanocyte suppression. These findings correlate with Ankad B et al 13 who reported hypopigmented patches as a frequent initial presentation in endemic regions. Erythematous lesions were noted in 28.8% (15/52) of cases, often associated with BL or LL, reflecting systemic immune compromise and higher bacillary loads (Figure 3).
Nerve thickening, seen in 9.6% (5/52), is a critical diagnostic clue, often correlating with advanced or longstanding disease where neural involvement is significant.
In 1966, Ridley-Jopling classified leprosy according to the clinical, bacteriological, immunological and histological categories into tuberculoid (TT), borderline tuberculoid (BT), mid borderline (BB), borderline lepromatous (BL) and lepromatous leprosy (LL) (Ridley & Jopling 1966) 8.
The present study was conducted to study the spectrum of types of leprosy and correlate the clinical phenotype with histopathological findings.
Clinical features indicate only the gross morphology of lesions which do relate to underlying pathological changes, while the histopathological features indicate the accurate response of tissue and bacteriological examination along with the bacillary load.
This study aims at analysing the newly diagnosed cases of leprosy attending our tertiary care centre in correlation with histopathology and bacteriological index (Table 2).
The most common index is Ridley's logarithmic measurement, which is based on the number of bacilli for the purpose of oil immersion, and graded as 9
|
Ridley-Jopling- Bacteriological index (BI) |
|
BI-6+ = more than 1000 bacilli in an average field, |
|
BI-5+ = 100 to 1000 bacilli in an average field, |
|
BI-4+ = 10 to 100 bacilli in an average field, |
|
BI-3+ = 1 to 10 bacilli in an average field, |
|
BI-2+ = 1 to 10 bacilli in 10 fields, and |
|
BI-1+ = 1 to 10 bacilli in 100 fields. |
|
BI-0 = No bacilli in 100 fields. |
At least 100 immersion oil smears should be checked before reporting bacterial index slides.
Amongst the 2-staining methods, Ziehl-Neelsen staining (ZN staining) / Fite-Faraco staining 14 (FF staining) sensitivity, positive predictive value and negative predictive value is maximum with Fite-Faraco stain as studied by Reja, et. al 15.
In the present study, the most common type of leprosy is Lepromatous leprosy (LL)-42.3%, followed by Borderline lepromatous (BL)-21%, Borderline Tuberculoid (BT)-15.4%, indeterminate leprosy (10%), and Mid borderline subtype (BB) and Tuberculoid leprosy (TT) (6%).
In the present study, the histopathological spectrum of leprosy showed that LL was the most prevalent type, accounting for 42.3% (22/52) of cases correlating with study done by Patel et al 16, Agarwal A, et al 17 showed LL was the most common histological type with 30% and 35.6% of cases respectively.
BL cases formed 21.1% (11/52), reflecting immune suppression and bacillary proliferation, often associated with higher rates of systemic manifestations. TT accounted for 15.4% (8/52) suggesting that TT is linked to good immunity with localized granulomas.
Overall concordance between clinical and histopathological classification had highest agreement observed in TT (96.2%) and BT, BB subtypes (94.2%) showing statistical correlation with concordance with studies of Atram, et.al 9, Kumar et al 10, Kini and Chaudhary 11 (Table 3, Table 4, Table 5).
These findings emphasize the importance of histopathology in confirming the clinical diagnosis and understanding disease progression suggesting that TT is characterized by well-formed granulomas with minimal bacillary presence, making it highly concordant with clinical findings, as observed in the study by Mukherjee et al 18.
These results underline the critical role of histopathological evaluation in enhancing diagnostic accuracy and guiding treatment.
Further discussing about the histopathological findings in each subtype in our study with images-
-
Tuberculoid leprosy: We have observed that the acid-fast bacilli are not seen. The epidermis is unremarkable. The deeper dermis shows granulomas, occasion giant cell, periappendageal and perineural lymphocytic infiltration (Figure 6, Figure 9), (Table 2).
-
Borderline tuberculoid: We have observed that the acid-fast bacilli are not seen in this type as well. The epidermis is atrophic and subepidermal zone is variably involved. Foreign body giant cells are seen most of the cases (Figure 7), (Table 2).
-
Mid Borderline: 80% the cases show acid-fast bacilli. Dermal oedema is noted. Few inflammatory cells are also observed (Table 2).
-
Borderline lepromatous: Majority of them showed the presence of acid-fast bacilli. The epidermis is atrophic. Grenz zone is seen. Dermis shows Virchow cells (macrophages), periappendageal and perineural lymphocytes in most of the cases (Figure 5), (Table 2).
-
Lepromatous leprosy: All the cases show acid-fast bacilli on Fite Faraco staining. The epidermis is thinned out with the flattening of rete ridges. There are seen foamy macrophages and focal plasma cells (Figure 4, Figure 8), (Table 2).
CONCLUSION
This study highlights the importance of histopathological evaluation in final diagnosis, offering critical insights into its diverse clinical and pathological spectrum. LL was the most prevalent histological type, followed by BL. A strong concordance was observed between clinical and histopathological diagnoses, particularly in TT cases with 96% agreement. Variations in concordance among other subtypes underscore the complexities of diagnosing borderline cases. These findings emphasize the necessity of combining clinical, histopathological, and immunological approaches to improve diagnostic accuracy and treatment strategies, ultimately aiding in the effective management and control of leprosy.
Continued surveillance and follow-up are very crucial steps given the declining yet persistent disease burden in our country.
References
-
2024. WHO. Weekly Epidemiological Record. Vol. 99. https://www.who.int/publications/journals/weekly-epidemiological-record
-
National Leprosy Eradication Programme – Annual Report for the year 2015-2016. https://dghs.gov.in/WriteReadData/userfiles/file/NLEP_Final_Annual_Report_2015-16.PDF
-
NLEP – Progress Report for the year 2010-11. Central Leprosy Division, Directorate General of Health Services, Nirman Bhawan, New Delhi – 110011, India. https://ghdx.healthdata.org/series/india-national-leprosy-eradication-programme-nlep
-
27 Jan 2023. WHO Expert Committee on Leprosy: seventh report. World Health Organization. https://apps.who.int/iris/handle/10665/42060
-
Katoch, Vishwa Mohan . 2024. Eradication of leprosy from India: Reflections on past, present & future. Indian Journal of Medical Research 159(1):1–5.
-
World Health Organization. Towards zero leprosy, global leprosy (Hansen's disease) strategy 2021-2030. https://www.who.int/publications/i/item/9789290228509
-
National Leprosy Eradication Programme. Central Leprosy Division, Directorate General of Health Sciences, Ministry of Health and Family Welfare, Government of India. National strategic plan and roadmap for Leprosy 2023-2027. https://dghs.gov.in/WriteReadData/userfiles/file/Leprosy%20New/NSP%20%20Roadmap%20for%20Leprosy%202023-2027.pdf
-
Ridley, D S & Jopling, W H . 1966. Classification of leprosy according to immunity. International Journal of Leprosy and Other Mycobacterial Diseases 34(3):255–273.
-
Kumar, Ankur, Negi, S & Vaishnav, Kusum . 2014. A study of Clinico-histopathological correlation of leprosy in a tertiary care hospital in western district of Rajasthan. Journal of Research in Medical and Dental Science 2(3):43–48.
-
Kini, Reshma & Choudhury, Hemangini . 2017. Clinico-pathological Correlation in Diagnosis of Hansen's Disease: A Histopathologist's Perspective. Journal of Interdisciplinary Histopathology 5:48–54.
-
Ghongade, Pravinkumar V, Atram, Manisha A & Gangane, Nitin M . 2020. A clinicohistopathological correlation of Hansen's disease in a rural tertiary care hospital of Central India. Journal of Global Infectious Diseases 12(4):191–196.
-
Archana, & Fernandes, Hilda . 2020. Clinico-Histopathological correlation in Hansen’s disease: A retrospective study. International Journal of Clinical and Diagnostic Pathology 3(3):168–172.
-
Ankad, Balachandra S, Sharma, Apoorva, Vinay, Keshavamurthy, Rathod, Santoshdev, Mehta, Hita, Bhat, Yasmeen Jabeen, Ashwini, P K, Jha, Abhijeet Kumar & Narang, Tarun . 2024. Dermatoscopic evaluation of leprosy: A multi-centre cross-sectional study. Indian Journal of Dermatology, Venereology and Leprology 90:486–493.
-
Fite, G L, Cambre, P J & Turner, M H . 1947. Procedure for demonstrating lepra bacilli in paraffin sections. Archives of pathology (Chic) 43(6):624–625.
-
A H Reja, N Biswas & S Biswas . 2013. Fite Faraco staining in combination with multiplex polymerase chain reaction: A new approach to leprosy diagnosis. Indian Journal of Dermatology, Venereology and Leprology 79:693–700.
-
Patel, Prashant R, Patel, Krutika, Vyas, Jhanvi & Bhagat, VM . 2022. A study of histopathological spectrum of leprosy at tertiary care hospital. Indian Journal of Pathology and Oncology 9(1):16–20.
-
Agarwal, A, Doberia, T & Dhruva, G . 2016. A Study of Histopathological Spectrum of Leprosy. International Journal of Scientific Research 5(11):133–135.
-
Mukherjee, Mala, Ghatak, Dhimoyee, Bhunia, Deblina, Das, Dipmala, Sinha, Ranwir K, Kumar, Nikhil & Roy, Asitava Deb . 2023. A study on the multidisciplinary diagnostic approach of leprosy: Can we prevent the recrudescence in the post-elimination Indian scenario? Journal of Family Medicine and Primary Care 12(9):2008–2013.
Copyright
©2025 (Cheruku & Shastry). This is an open-access journal, and articles are distributed under the terms of the Creative Commons Attribution License CC-BY 4.0. (https://creativecommons.org/licenses/by/4.0/) which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited.
Cite this article
Cheruku S, Shastry S. Hansen’s Disease- A Comprehensive Study Through the Lens of Histopathology and Clinical Correlation: In a Teri-
tiary Care Centre. Perspectives in Medical Research. 2025;13(3):163-169 DOI: 10.47799/pimr.1303.25.54