Volume: 13 Issue: 3
The Cytological Evaluation of Thyroid Lesions with Emphasis on the Bethesda System for Reporting of Thyroid Cytopathology in Correlation to Histopathology – A Descriptive Study
Year: 2025, Page: 157-162, Doi: https://doi.org/10.47799/pimr.1303.25.20
Received: June 19, 2025 Accepted: Oct. 25, 2025 Published: Dec. 31, 2025
Abstract
Introduction : Fine needle aspiration cytology (FNAC) of the thyroid gland is a first-line diagnostic test for the preoperative diagnosis of a solitary thyroid nodule. It is cost effective and minimally invasive technique. The 2023 Bethesda system for reporting thyroid cytopathology (TBSRTC) simplifies the system by having one name for each category. Aims : To categorize various thyroid lesions as per TBSRTC 2023 and correlate the Fine needle aspiration cytology diagnosis with histopathological findings. Material and Methods: The descriptive study was conducted in a tertiary care hospital over a period of two years. Total 97 patients underwent fine needle aspiration cytology of thyroid lesions after taking detailed clinical history. The cytomorphological diagnosis was given and then subsequent biopsy/thyroidectomy specimens were received. Finally, cytohistopathological correlation was done. Results: Out of total 97 cases of thyroid lesions, 7 cases (7.21%) were reported as category I, 71 cases (73.19%) as category II as benign lesions, 2.06% as category III, 8.24% cases as category IV, 5.15% as category V, 4.12% as category VI as malignant. Majority of cases were in 31-40 years of age group. Only 63 cases were available for histopathological examination. Conclusion: The correlation between Bethesda System-guided cytology and histopathology elucidates the refinement of thyroid lesion diagnosis.
Keywords: Bethesda, Cytology, Thyroid
INTRODUCTION
The evaluation of thyroid lesions through cytology stands as a pivotal component in diagnosing thyroid disorders. With an emphasis on the Bethesda System for Reporting Thyroid Cytopathology (TBSRTC), this method offers a standardized approach to interpreting fine-needle aspiration (FNA) biopsies of thyroid nodules, aiding in effective communication between clinicians and pathologists. 1
FNAC is a cost effective and a minimally invasive technique. It also avoids the rate of unnecessary surgery done in the case of benign thyroid nodules. 2
The Bethesda system for Thyroid Cytopathology (TBSRTC) was introduced in 2007 at the National Cancer Thyroid FNA state of science conference in Bethesda, Maryland. 3
The TBSRTC classifies thyroid FNA results into six diagnostic categories guiding subsequent clinical management based on the risk of malignancy associated with each category. 1, 4
TBSRTC 2023 recommends a single designation for each of the 6 categories, discontinuing the use of previously used terms like ‘‘unsatisfactory,’’ ‘‘follicular lesion of undetermined significance,’’ and ‘‘suspicious for a follicular neoplasm.’’
TBSRTC 2023 recommends use of following 6 reporting categories: (i) nondiagnostic (ii) benign; (iii) atypia of undetermined significance (AUS) (iv) follicular neoplasm (FN) (v) suspicious for malignancy (SFM) and (vi) malignant (Table 1).
Table 1: The Bethesda system for reporting thyroid cytopathology: implied risk of malignancy (ROM) and recommended clinical management. 5
|
Diagnostic Category |
Risk of malignancy (range) |
Usual Management |
|
I. Non – diagnostic |
13(5-20) |
Repeat with USG |
|
II. Benign |
4(2-7) |
Clinical and sonographic follow-up |
|
III. Atypia of undetermined significance |
22(12-30) |
Repeat FNA, molecular testing, diagnostic lobectomy |
|
IV. Follicular neoplasm |
30(23-34) |
Molecular testing, diagnostic lobectomy |
|
V. Suspicious for Malignancy |
74(67-83) |
Molecular testing, lobectomy or near-total thyroidectomy |
|
VI. Malignant |
97(97-100) |
Lobectomy or near-total thyroidectomy |
This evaluation bridges the gap between cytology and histopathology, establishing correlation that significantly impact patient care. Histopathology serves as the gold standard for definitive diagnosis. The correlation between cytological findings and subsequent histopathological examination offers a comprehensive understanding of the disease spectrum, enhancing diagnostic accuracy and treatment planning. 6
The aim of present study is to categorize the thyroid lesions according to the Bethesda system (2023) in correlation to histopathology.
MATERIAL AND METHODS
A cross-sectional descriptive study was conducted in the Department of Pathology Government Medical college, Dhule from Jan 2022 – Dec 2023. The present study included 97 cases presenting with thyroid lesions referred to cytology department. Detailed clinical examination was performed, and clinical history were taken from each patient. After explanation of procedure and taking informed consent of patient, FNAC was performed by using 22/23G needle, with or without the use of syringe for aspiration. Smears were prepared then fixed in methanol and stained by Hematoxylin and Eosin and Papanicolaou stain. Smears were evaluated according to Bethesda system of reporting. The six categories of TBSRTC (2023) are as follows I. ND (non-diagnostic), II. Benign, III. AUS, IV. FN, V. Suspicious for malignancy and VI. Malignant.
Subsequent biopsies/thyroidectomy specimens sent from surgical department were grossed, processed by paraffin embedding and stained with Hematoxylin and Eosin.
Inclusion criteria - All patients with thyroid lesions referred by clinician and surgeon for FNAC irrespective of gender and age.
RESULT
The present study included 97 cases of thyroid lesions which underwent FNAC were performed over a period of 2 yrs. The study included 21 cases of male (21.64%) and 76 cases of female (78.35%). The male to female ratio of 1:3.62 was observed in our study. The maximum number of patients were in the age group of 31-40yrs (31.95%) (Table 2).
Table 2: Age wise distribution of cases
|
Age group (Years) |
Number of patients |
Percentage (%) |
|
0-10 |
02 |
2.06% |
|
11-20 |
08 |
8.24% |
|
21-30 |
15 |
15.46% |
|
31-40 |
31 |
31.95% |
|
41-50 |
13 |
13.40% |
|
51- 60 |
12 |
12.37% |
|
61-70 |
14 |
14.43% |
|
71- 80 |
02 |
2.06% |
The cytopathological evaluation was done and all cases were categorized according to TBSRTC. Out of total 97 cases, 71 (73.19%) cases were present in category II as benign lesions whereas category VI malignant lesions seen in 4 cases (4.12%). 07 (7.21%) cases were in the non-diagnostic category, 02 (2.06%) cases were in atypia of undetermined significance, 8 (8.24%) cases in follicular neoplasm. 5 (5.15%) cases belonged to suspicious for malignancy (Table 3).
Table 3: Distribution of cases according to Modified Bethesda system
|
Cytological categories |
No. of cases |
Percentage |
|
I. Non – diagnostic |
07 |
7.21 % |
|
II. Benign |
71 |
73.19 % |
|
III. AUS |
02 |
2.06 % |
|
IV. FN |
08 |
8.24 % |
|
V. SFM |
05 |
5.15 % |
|
VI. Malignant |
04 |
4.12 % |
Total number of benign lesions were 71, out of which 51 cases were colloid goiter, 11 cases were colloid goiter with cystic change, 2 cases were thyroglossal cyst, 5 cases were Hashimoto thyroiditis, and 2 cases were lymphocytic thyroiditis (Figure 1).
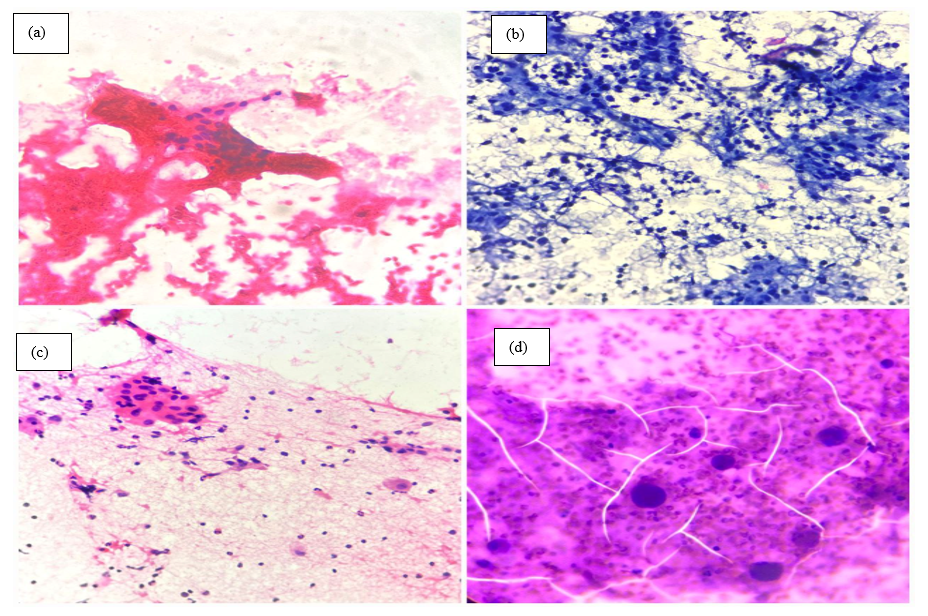
Figure 1: (a) Cytological smears of Colloid goitre showing abundant colloid and follicular epithelial cells (H&E 10x). (b) Cytological smears of Hashimoto thyroiditis showing sheets of follicular epithelial cells admixed with Hurthle cells and lymphocytes. (Papanicolaou stain 10x). (c) Cytological smears of Lymphocytic thyroiditis showing cluster of follicular epithelial cells and moderate lymphocytic infiltration (H&E 10x). (d) Cytological smears of Thyroglossal cyst showing foamy histiocytes, abundant colloid and squamous cell (H&E 10x)
Category V assigned as suspicious for malignancy reported 4 cases as papillary carcinoma and only one case was reported as medullary carcinoma. Out of 4 cases of category VI as malignant, two cases were papillary carcinoma, one case was medullary carcinoma, and one case was anaplastic carcinoma (Table 4) (Figure 2).
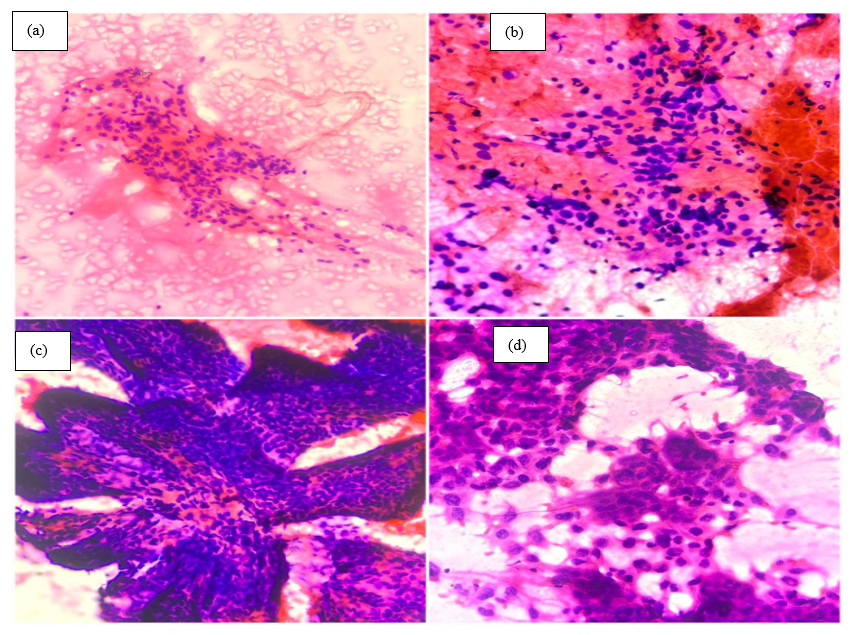
Figure 2: (a) Cytological smears of Follicular neoplasm - The nuclei are normal-sized and round, with the chromatin clumpy/slightly hyperchromatic and inconspicuous nucleolus (H&E 10x). (b) Cytological smears of Suspicious for malignancy. These representative microfollicular groups display nuclear enlargement, variable chromatin pallor. (H&E 40x). (c) Cytological smears of Papillary carcinoma - Branching papillary tissue fragment with fibrovascular core with nuclear crowding and overlapping (H&E 10x). (d) Cytological smears of Anaplastic thyroid carcinoma- large, bizzare, malignant tumor cell with nuclear pleomorphism, irregular nuclear membrane, giant cells and a prominent nucleolus with several intranuclear pseudoinclusion. (H&E 40x)
Table 4: Distribution of cases according to Modified Bethesda system
|
Cat |
Diagnostic category |
Cases |
Total no. of cases |
|
I |
Non-diagnostic |
Acellular (03) Haemorrhagic (04) |
07 |
|
II |
Benign |
Colloid goiter (51) Colloid goiter with cystic changes (11) Thyroglossal cyst (2) Hashimoto thyroiditis (5) Lymphocytic thyroiditis (2) |
71 |
|
III |
AUS |
AUS (2) |
02 |
|
IV |
FN |
Follicular neoplasm (8) |
08 |
|
V |
SFM |
Suspicious for papillary carcinoma (4) Suspicious for Medullary carcinoma (1) |
05 |
|
VI |
Malignant |
Papillary carcinoma (2) Medullary carcinoma (1) Anaplastic carcinoma (1) |
04 |
Out of 97 cases, histopathological correlation was available in 63 cases. Out of 71 cases of category II, only 47 cases were available for histopathological follow up, out of which 31 cases were colloid goiter, 12 cases reported as colloid goiter with cystic changes, 2 cases reported as Hashimoto thyroiditis and 2 cases diagnosed as thyroglossal cyst. one out of 6 cases of category IV were turned out to be malignant on histopathological examination and risk of malignancy was 16.6%. 2 out of 3 cases belonging to category V of suspicious of malignancy were reported as a malignancy on histopathological examination and risk of malignancy was 67%. All of the cases of category VI were reported as malignancy on histopathological examination and risk of malignancy was 100% (Table 5) (Figure 3).
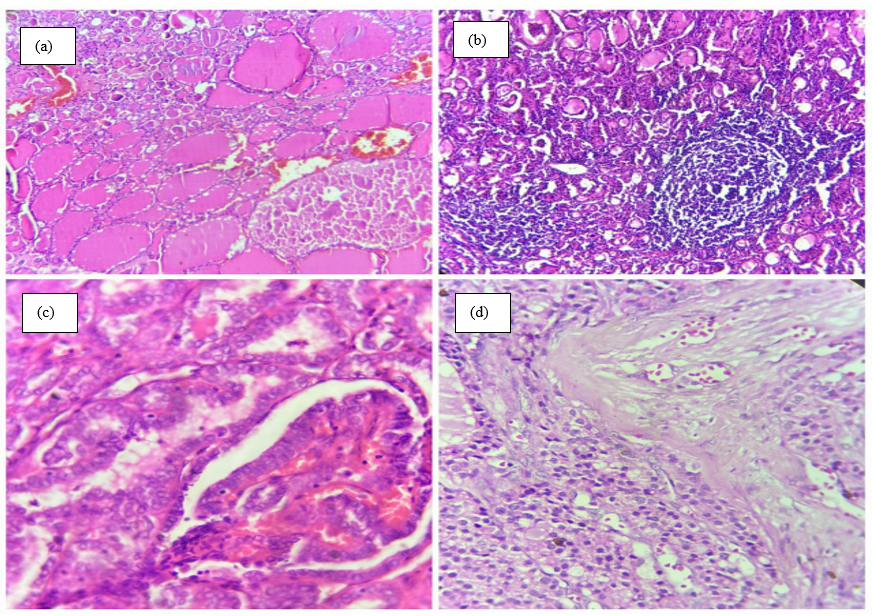
Figure 3: (a) Histopathological section of colloid goiter shows variable sized thyroid follicles filled with eosinophilic colloid material (H&E 10x). (b) Histopathological section of Hashimoto’s thyroiditis shows thyroid parenchyma with lymphocytic infiltration in the form of lymphoid follicles (H&E 10x). (c) Histopathological section of papillary carcinoma shows tumor tissue composed of papillae with a fibrovascular core (H&E 40x). (d) Histopathological section of follicular carcinoma shows tumor tissue with follicular architecture and surrounding fibrous capsule along with capsular invasion (H&E 40x)
Table 5: Malignancy risk for each Bethesda category after histopathology
|
Sr. No |
Bethesda system diagnosis of FNAC |
Diagnosis on Histopathology |
No of the cases turned out to be malignant |
Risk of malignancy (%) |
|
1 |
Non-diagnostic (07) |
Colloid goiter (5) |
0 |
- |
|
2 |
Benign (71) |
Colloid goiter (31) Colloid goiter with cystic change (12) Thyroglossal cyst (2) Hashimoto thyroiditis (2) |
0 |
- |
|
3 |
AUS (2) |
- |
0 |
|
|
4 |
FN (8) |
Follicular adenoma (4) Multinodular goiter (1) Follicular carcinoma (1) |
1 |
16.6% |
|
5 |
SFM (5) |
Multinodular goiter (1) Papillary carcinoma (2) |
2 |
67% |
|
6 |
Malignant (4) |
Papillary carcinoma (2) |
2 |
100% |
DISCUSSION
Accurate classification via Bethesda System categories aids in risk stratification, refining treatment strategies. Understanding discrepancies informs improved patient management, minimizing unnecessary surgeries. This correlation serves as a crucial guide for clinicians, emphasizing the necessity of comprehensive evaluations for optimal patient care. 4
The BSRTC categorizes thyroid nodules in six categories; hence, appropriately triaging patients with malignant nodules for timely surgical intervention. 7
In the BSRTC, surgery is not recommended for ND, benign, and AUS category. In cases with FN/SFN, SFM and malignant categories, and excision of nodules or partial/complete thyroidectomy was performed as per the BSRTC recommendations.
The present study was carried out over a period of two years to categorize the cytology reports according to TBSRTC and correlated histologically for malignancy risk. The FNAC was performed on 97 patients and only 63 cases were followed by histopathological examination.
Majority of patients were female with M:F was 1:3.62 in the present study which was in close comparison with that of Mittal N et al. 8 In the present study, the age range from 8 years to 74 years and maximum numbers of patients were in the age group of 31-40 years which was in concordance with Mittal N et al 8 , Choudhary S et al 9 , Kumar G et al 10 , Agrawal R et al 11 .
In the third edition of TBSRTC, “Unsatisfactory” is removed from the name of the category. Non-diagnostic category included cyst fluid only, virtually acellular specimen, other (obscuring blood, clotting artifact, drying artifact).
In our study 07 cases were under category I as nondiagnostic which was in close comparison to Patel K et al. 12 All cases were reported as acellular smears because of absence of colloid, lack of follicular epithelial cells and presence of haemorrhage. Later, on repeat aspiration, 02 cases remained nondiagnostic while 5 cases were diagnosed as colloid goiter, both on cytology and histopathology. Thus, a smear is considered adequate only when if it contains a minimum of six groups of well-preserved follicular cells containing at least 10 cells per group.
The most common finding was benign lesion category II in which colloid goiter was predominant findings on cytology and histopathology. Similar findings reported by Patel K et al 12 , Anand B et al 13 , Kumar G et al 10 , Reddy P et al. 14
The third edition of TBSRTC simplified the terminology and removed “follicular lesion of undetermined significance (FLUS)” from the diagnostic term. It also re-organized AUS scenarios and formalized subclassification of AUS as AUS-nuclear atypia and AUS-other. 15
For this entity to remain a valid and valuable category, AUS should not be over-used. 16
Cases with scant follicular groups trapped in fibrin clots with crowded architecture or focal nuclear pallor should be called non-diagnostic instead of AUS. A cellular aspirate with predominant benign findings and only focal microfollicles should be called benign, not AUS. AUS serves as a good quality measure. The second edition of TBSRTC proposes that AUS should remain < 10% of all thyroid diagnoses. Alternatively, an AUS/malignant ratio not exceeding 3 is suggested as a good quality measure for a cytopathology lab. 17
The least number of cases were in category III atypia of undetermined significance which was again comparable to the study done by Reddy P et al 14 and kumar G et al. 10
In our study 08 cases were diagnosed as follicular neoplasm category IV which was comparable to the study done by Yassa et al 18 and Jo et al. 7 Majority of cases in SFM and malignancy category were reported as papillary carcinoma of thyroid which was in concordance with the studies done by Kumar G et al 10 and AI Dawish MA et al. 19
The percentage of malignant cases in the present study was 4.12% which was comparable to that of Reddy P et al 14 , Mittal N et al 8 , Kumar G et al 10 and Mondal et al. 20 Cytohistopathological correlation was done in 63 cases only, of which majority of lesions were benign. Malignancy risk of different category was calculated and compared with other studies. 7, 10
CONCLUSION
The correlation between Bethesda System-guided cytology and subsequent histopathology in thyroid lesions highlights the diagnostic accuracy. The potential benefits of FNAC is reducing unnecessary surgery for benign lesions. The advantage of TBSRTC has implied risk of malignancy which helps enhancing diagnostic accuracy and refining management strategies.
References
-
Cibas, E S & Ali, S Z . 2009. The Bethesda System For Reporting Thyroid Cytopathology. American Journal of Clinical Pathology 132(5):658–665.
-
Somma, J, Schlecht, N F, Fink, D, Khader, Samer N, Smith, Richard V & Cajigas, Antonio . 2010. Thyroid fine-needle aspiration cytology: Follicular lesions and the gray zone. Acta Cytologica 54(2):123–131.
-
Baloch, Zubair W, LiVolsi, Virginia A, Asa, Syl L, Rosai, Juan, Merino, Maria J, Randolph, Gregory, Vielh, Philippe, DeMay, Richard M, Sidawy, Mary K & Frable, William J . 2008. Diagnostic terminology and morphologic criteria for cytologic diagnosis of thyroid lesions: A synopsis of the National Cancer Institute Thyroid Fine‐Needle Aspiration State of the Science Conference. Diagnostic Cytopathology 36(6):425–437.
-
Bongiovanni, Massimo, Spitale, Alessandra, Faquin, William C, Mazzucchelli, Luca & Baloch, Zubair W . 2012. The Bethesda System for Reporting Thyroid Cytopathology: A Meta-Analysis. Acta Cytologica 56(4):333–339.
-
Ali, Syed Z, Baloch, Zubair W, Cochand-Priollet, Beatrix, Schmitt, Fernando C, Vielh, Philippe & VanderLaan, Paul A . 2023. The 2023 Bethesda System for Reporting Thyroid Cytopathology. Thyroid 33(9):1039–1044.
-
Afroz, N, Kayani, N & Hasan, S H . 2002. Role of fine needle aspiration cytology in the diagnosis of palpable thyroid lesions. Indian Journal of Pathology and Microbiology 45(3):241–246.
-
Jo, Vickie Y, Stelow, Edward B, Dustin, Simone M & Hanley, Krisztina Z . 2010. Malignancy Risk for Fine-Needle Aspiration of Thyroid Lesions According to The Bethesda System for Reporting Thyroid Cytopathology. American Journal of Clinical Pathology 134(3):450–456.
-
Mittal, Navkirti, Selhi, Pavneet, Kaur, Harpreet, Mittal, Ankur, Nagiraj, Anita, Singh, Aminder & Sood, Neena . 2018. Cytomorphological analysis of categories in the Bethesda system and its accuracy in predicting thyroid neoplasms. Thyroid Research and Practice 15(2):84–88.
-
Choudhury, Sampa, Deshpande, Archana H & Gargade, Chitrawati B . 2020. The Bethesda system for reporting thyroid FNAC: A cytohistological correlation in a newly established institute. Indian Journal of Pathology and Oncology 5(4):650–655.
-
Kumar, Gaurav, Sharma, Ritu, Jaiswal, Saurabh Kumar & Pal, Desh . 2022. Thyroid Lesions: Cytomorphological Classification of Fine Needle Aspiration Cytology into Modified Bethesda System: A 3-Year Retrospective Study. Bengal Journal of Otolaryngology and Head Neck Surgery 30(1):108–115.
-
Agrawal, Ranjan, Saxena, Manoj & Kumar, Parbodh . 2015. A Study of Fine Needle Aspiration Cytology of Thyroid Lesions with Histopathological Correlation. Indian Journal of Pathology and Oncology 2(4):277–283.
-
Patel, Keval A, Anandani, Garima, Sharma, Bhawana S & Parmar, Riddhi A . 2023. Study of Fine Needle Aspiration Cytology (FNAC) of Thyroid Gland According to the Bethesda System. Cureus 15(4):e37371.
-
Anand, Bakiarathana, Ramdas, Anita, Ambroise, Marie Moses & Kumar, Nirmal P . 2020. The Bethesda System for Reporting Thyroid Cytopathology: A Cytohistological Study. Journal of Thyroid Research 2020:1–8.
-
Reddy, Purushotham, Prakash, Akina & Giriyan, Sujata S . 2017. Evaluation of Bethesda system for reporting thyroid cytology with histopathological correlation. International Journal of Research in Medical Sciences 6(1):247–252.
-
Han, Min & Fan, F . 2023. Bethesda System for Reporting Thyroid Cytopathology–An Updated Review. Journal of Clinical and Translational Pathology 3(2):84–98.
-
Kim, Teresa H & Krane, Jeffrey F . 2022. The evolution of “atypia” in thyroid fine-needle aspiration specimens. Diagnostic Cytopathology 50(4):146–153.
-
Krane, J F, Vanderlaan, P A, Faquin, W C & Renshaw, A A . 2012. The atypia of undetermined significance/follicular lesion of undetermined significance:malignant ratio: a proposed performance measure for reporting in The Bethesda System for thyroid cytopathology. Cancer Cytopathology 120(2):111–6.
-
Yassa, Leila, Cibas, Edmund S, Benson, Carol B, Frates, Mary C, Doubilet, Peter M, Gawande, Atul A, Moore, Francis D, Kim, Brian W, Nosé, Vânia, Marqusee, Ellen, Larsen, P Reed & Alexander, Erik K . 2007. Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer 111(6):508–516.
-
Dawish, Mohamed Abdulaziz Al, Robert, Asirvatham Alwin, Muna, Aljuboury, Eyad, Alkharashi, Ghamdi, Abdullah Al, Hajeri, Khalid Al, Thabet, Mohammed A & Braham, Rim . 2017. Bethesda System for Reporting Thyroid Cytopathology: A three-year study at a tertiary care referral center in Saudi Arabia. World Journal of Clinical Oncology 8(2):151–157.
-
Mondal, Santosh Kumar, Sinha, Simanti, Basak, Bijan, Roy, Dipanwita Nag & Sinha, Swapan Kumar . 2013. The Bethesda system for reporting thyroid fine needle aspirates: A cytologic study with histologic follow-up. Journal of Cytology 30(2):94–99.
Copyright
©2025 (Damle) et al. This is an open-access journal, and articles are distributed under the terms of the Creative Commons Attribution License CC-BY 4.0. (https://creativecommons.org/licenses/by/4.0/) which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited.
Cite this article
Damle RP, Patil BM, Thakare SS, Vasaikar MS, Pandhare V. The Cytological Evaluation of Thyroid Lesions with Emphasis on the Bethesda System for Reporting of Thyroid Cytopathology in Correlation to Histopathology – A Descriptive Study. Perspectives in
Medical Research. 2025;13(3):157-162 DOI: 10.47799/pimr.1303.25.20